Caesarean section is a popular operation today. Back in the 70s of the last century, the total share of operative births was no more than 2%, and now it has grown to almost 20%. Every fifth baby is born through a cesarean section. This is due to the ecological situation, and to the fact that women have become less mobile, weaker than 40-50 years ago, the proportion of IVF has increased and more and more women are thinking about offspring for the first time after 35 years. Therefore, a planned caesarean section is no longer surprising.
In this article we will talk about how and when a cesarean section is performed, what are the features of a planned operation.

Types of surgery and indications for it
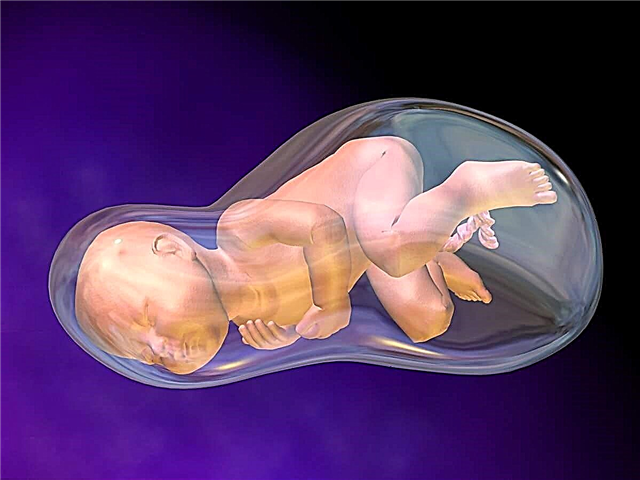
Caesarean section is a delivery operation that involves removing the baby and the placenta through an incision in the abdomen. The operation can be carried out urgently - due to vital indications and unforeseen circumstances that arose suddenly and made physiological childbirth impossible or extremely dangerous. In a planned manner, the operation is performed in case of detection of circumstances that are direct or relative indications for operative delivery during pregnancy.
A planned cesarean differs from an emergency one in the absence of haste, in the presence of thorough preparation. Complications after elective surgery are less common. Also, different types of surgery imply different indications. If an emergency cesarean section is performed mainly with weakness of the labor forces, the absence of the effect of stimulation in one of the stages of the onset of physiological labor, with placental abruption prematurely or with acute fetal hypoxia that threatens the baby's life, then the indications for elective surgery are more extensive.

A planned cesarean is done in the following cases.
- "Child's place" is located below the normal level, there is presentation. The placenta completely or partially closes the internal pharynx, there is a high probability of bleeding.
- A scar on the uterus from a previous cesarean or other operation on the uterus can be dangerous in terms of the possibility of uterine rupture during labor.
- Consistent scar, but two or more caesarean in history.
- Obstacles that can be considered mechanical. Normal childbirth will be hampered by the narrow pelvis of the woman in labor, injured or deformed bones and joints of the pelvis, tumors of the uterus, ovaries, multiple polyps.
- The discrepancy of the pubic bones is symphysitis.


- Unsuitable presentation of the fetus for physiological childbirth (these include the pelvic, oblique or transverse, as well as the buttock-leg position of the baby relative to the exit from the uterus), an aggravating factor is the alleged large weight of the fetus (more than 3600 g).
- Pregnancy with twins, if with it one of the children lies in the wrong presentation or there is a baby in the pelvic position, which is closer to the exit from the uterus.
- Pregnancy with monozygous twins, if children are located inside one fetal bladder.
- Pregnancy (including multiple pregnancy), which became possible as a result of a successful treatment cycle of in vitro fertilization.
- Injured cervix, scars on it and in the vagina after a previous difficult birth.
- Severe delay in fetal development, a significant delay in the development of the baby in terms of timing.


- Prolonged pregnancy - after 42 weeks, if stimulation was ineffective.
- Severe gestosis.
- Diseases in the mother in which it is strictly forbidden to push - myopia, cardiovascular problems, kidney transplanted.
- The state of chronic oxygen starvation in the fetus.
- Herpes of the genital type.
- Problems with hemostasis in a woman or child.
- Some fetal malformations.


At the request of a woman in labor, a caesarean section in Russia is performed only in some paid clinics. An elective cesarean section can cost up to half a million rubles. Free of charge, that is, according to the policy of compulsory medical insurance, the operation is carried out by maternity hospitals, perinatal centers only if there are compelling medical reasons why surgical delivery is more optimal than physiological. This is associated with a high risk of complications, which the woman and the baby will not be exposed to if the potential risk outweighs the possible benefits of the intervention.

When do they do it?
Considering that doctors need to collect as much information as possible about the condition of the future woman in labor and her baby, the decision on the need and timing of a caesarean section is routinely made at 34-35 weeks of pregnancy. This primarily applies to situations in which the baby is located in the uterus in a pelvic or other abnormal presentation, when it is imperative to find out its estimated weight. If during pregnancy from the first months there are certain indications, for example, a third or fourth surgical delivery is coming, the question of the appointment of an operation is not raised, it is resolved by default.
There is an opinion that the caesarean, which they begin to do after a woman's independent contractions start, is more natural and closer to physiological childbirth. Experienced and prudent surgeons prefer to perform the operation before the onset of regular labor pains. The calmer the muscles of the uterus, the less likely postoperative complications are.

The Russian Ministry of Health ordered a planned operation after 39 weeks. Theoretically, the baby is viable earlier, after 36-37 weeks, but in practice, the risks of developing respiratory failure remain due to the possible small amount of surfactant in the lungs. Therefore, at the first birth, the operation is performed at a period of 39-40 weeks. A second CS may be performed at 39 weeks, and a third at 38-39 weeks. The difference is due to the fact that subsequent bearing of a fetus with a scar on the uterus is associated with an increased risk of scar dehiscence at the later stages, the likelihood of an early onset of contractions is higher.
The date of the operation is set not only taking into account the interests of the expectant mother, but also taking into account the interests of the child.
If there are signs of his trouble, the timing of a planned surgical delivery may well be moved a few days earlier. Planned surgeries are not performed on weekends, even if the patient gives birth for a fee, until the contract for the provision of paid medical services.

The estimated date of the operation may change for various reasons. In particular, the intervention can be carried out earlier if a woman shows signs of the readiness of the cervix for the onset of labor, when the mucous plug leaves or the amniotic fluid leaks, if there are warning signs of a threatening rupture of an old scar on the uterus, if the woman's condition has worsened due to gestosis , if the baby has oxygen starvation according to the results of CTG and ultrasound, the umbilical cord entwined around the neck.
The patient receives a referral to the maternity hospital in the antenatal clinic at 38 weeks pregnant, since hospitalization before the planned operation is done well in advance.


Preparing for surgery
Before a planned surgical delivery, a woman is placed in a maternity hospital at 38-39 weeks of gestation. You need to go to the hospital in order to prepare for the upcoming operation as best as possible. Preparation at the maternity hospital will include the next general examination - blood and urine tests, ultrasound, CTG.
A woman will definitely undergo a coagulogram - a blood test for coagulation factors. This is important for planning your surgery. She will also have a conversation with an anesthesiologist when she will have to decide on the type of anesthesia. The bag, which the woman collects in advance in the maternity hospital, before the cesarean section must contain a set of elastic bandages for bandaging the legs in order to avoid thrombosis during and after surgery, or compression stockings for the same purposes. You can take a disposable machine with you, it will come in handy on the day of the operation.
In the morning, a woman is lifted up early, an enema is done to cleanse the intestines (this will help later a faster contraction of the uterus), her pubis is shaved to prevent hair from getting on the wound surfaces. Scheduled operations begin in the morning.

Narcosis
Anesthesia can be of three types. The most widespread in recent years have received epidural and spinal anesthesia. With these methods, anesthetics and muscle relaxants are injected into the epidural space of the spinal column or into the subarachnoid space of the spine. For the injection, the anesthesiologist uses a long, thin needle, the injection is carried out in a sitting position or lying on its side. The puncture site is the lumbar spine. The needle should go between the vertebrae. Pain relief occurs within 15 minutes with epidural anesthesia and almost immediately with spinal anesthesia.
Lower body becomes numb and loses sensitivity. Doctors can proceed to the operation, and the anesthesiologist leaves a catheter at the site of the lumbar puncture, through which, if necessary, he can administer additional doses of pain medications if the operation is delayed. The woman is fully conscious, she can communicate with doctors, see a wonderful moment - the birth of a baby, and there is also an opportunity to immediately attach the baby to the breast right on the operating table.

General anesthesia involves immersing a woman in deep medication sleep. In the operating room, she is given an intravenous anesthetic, she falls asleep, after which a tracheal tube is inserted and connected to an artificial respiration apparatus. Drugs to maintain narcotic sleep can be given in steam form through a tube, or they can be given intravenously through a catheter left there. A woman can neither see nor hear anything in a state of general anesthesia.
General anesthesia is prescribed when there are certain contraindications to epidural or spinal anesthesia, as well as in cases where the woman herself insists on deep medication sleep during the operation - not everyone likes to hear and watch how surgeons work.

Execution technique
They try to do a planned operation with the least damage to the beauty of the female body. The incision is made horizontal; its length does not exceed 10 centimeters. The incision line runs parallel to the pubis. After the incision of the skin, adipose tissue, and also the muscle tissue of the aponeurosis, the surgeon must protect the muscles and bladder from possible accidental injury with a scalpel during manipulations on the uterus. He takes them to the sides and fixes them with clamps.
The uterus is dissected in the lower uterine segment. This segment stretches the least, and therefore preserves the prospect of becoming a mother for a woman several more times. Having opened the uterine cavity, the doctor opens the fetal bladder, drains the amniotic fluid, grabs the baby's head in the back of the head with his hand and gently removes the baby into the light. The umbilical cord is cut.
Then the placenta is manually removed and sutured in reverse order. First - on the uterus, then on the muscle tissue. Last of all, the skin on the abdomen is sutured. From the moment of the beginning of the operation to its end in the normal mode, usually no more than 40 minutes pass.
Features of reoperation
Reoperation may take slightly longer than the first. This is due to the need to excise the old scar on the uterus and form a new suture. The fact is that the subsequent surgical delivery is carried out along the line of the old scar. This rule is valid in 99% of cases, only sometimes you have to deviate from it, if there are certain reasons.
With a second birth or a third cesarean section, some women agree to ligation of the fallopian tubes in order to exclude the likelihood of a subsequent pregnancy, since each subsequent proceeds with increasing risks. This procedure adds about 10 minutes more to the operation time, so a repeat surgical delivery can last up to 50-60 minutes.

Rehabilitation
Much in the future well-being of the newly-made mother will depend on how correctly the rehabilitation is organized. In the first hours after the operation, the woman in labor is in a special intensive care unit, where doctors are closely watching her. Everything is important - how a woman will come out of anesthesia, what will be the blood pressure, body temperature, how quickly the reverse involution of the uterus (contraction) will begin.
Already in the intensive care unit, a woman begins to be injected with contraction drugs, the task of which is to strengthen uterine contractions. Pain relievers are given without fail, antibiotics can be prescribed if doctors have reason to assume a high risk of postoperative complications.
After 5-6 hours, the woman is transferred to the general ward. There, after another couple of hours, she can begin to roll over on one side, sit down, gradually get up and take the first steps. The earlier the parturient woman rises and begins to move moderately, the better for uterine contraction, for faster recovery.

Early attachment of the baby to the breast is encouraged. The earlier the baby begins to suck it, the faster the hormonal balance in the woman's body will normalize, the more actively oxytocin will be produced, the uterus will contract better.
In the first three days, the woman is prescribed a special diet. On the first day, only water without gas, the next day - broth, jelly, compote without sugar, homemade white crackers without spices and salt. On the third day, you can eat porridge, vegetable purees. On the fourth day, the woman is transferred to a common table, but it is recommended to avoid foods that can cause constipation, gas in the intestines, and bloating. Discharged after a planned caesarean section in the absence of complications on the fifth day. The woman removes the stitches in the antenatal clinic at the place of residence for 7-8 days.

Reviews
According to the reviews of women that they left on the Internet on the pages of thematic forums, a planned cesarean section is a good way to choose the date of birth of your own baby. If there is no indication for a shift in terms, the woman is given such an opportunity, limiting it to one week. Knowing when the baby will be born makes it possible to choose a name in advance according to the Holy Calendar, as well as mentally and physically prepare for this important event in the life of the family.
For women who are scheduled to have a caesarean section, it is important to choose in advance the maternity hospital or perinatal center where she would like to be operated on. After that, in the selected maternity hospital, you need to sign an exchange card with the chief physician or his deputy for the medical part (chief medical officer). Then, no matter what happens while waiting for the date of hospitalization, the ambulance will take the patient to the very hospital that will be indicated on the exchange card. Otherwise, you may get into another obstetric institution, which will be on duty.

Quite often, women who are about to have their first planned delivery wind themselves up to neurosis - they watch a video of the operation, read about its possible complications and a terrible way out of anesthesia. After leaving their own experience behind, most admit that the rumors and fears were clearly exaggerated. Modern medications do not make anesthesia difficult and painful, the way out of it is easier, even if you did general anesthesia.
By the way, opinions on the choice of anesthesia are also controversial.Many women prefer the general one, because they already have experience with an epidural and know that with it, not all sensitivity disappears, and listening to doctors' conversations and the clang of instruments is not at all pleasant. A big plus of a planned operation is the postoperative suture, which after six months decreases to 4-5 centimeters, brightens and becomes almost invisible.
In an emergency operation, the seams are less accurate, moreover, the operation can be performed in a corporal way - a vertical incision from the navel to the pubis. It will be impossible to hide such a scar behind an elastic band of panties, and complications are more common.

Experienced mothers advise a woman who is just preparing for a COP to discuss with the doctor in advance all the nuances of the upcoming operation and ask all questions. Then there will be less worries.
For information on when a cesarean section is recommended, see the next video.