The term "stridor" is not familiar to everyone. Under this concept in the medical literature it is customary to understand noisy, rough, wheezing breathing. Stridor breathing is the main manifestation of laryngeal pathology.
Stridor is not an independent disease, but is considered a symptom of any disease manifested by airway stenosis.
What causes stridor?
This question often arises before parents. Indeed, before treatment, it is always important to identify the main cause of the development of a pathological symptom.
Predisposing Airway Features in Children
Of course, stridor breathing is more likely to occur in young children. Because the anatomy of the upper respiratory tract is imperfect and there are some peculiarities. The larynx in children has a small gap. But the main mechanism for the development of stridor breathing is the appearance of turbulent air flows after it passes through the narrowed lumen of the larynx.
But it is important to note that not all children have pathological stridor. The situation worsens with abnormalities in the development of the upper respiratory tract. If there is a weakness of the cartilaginous elements of the larynx, then the sagging of such cartilage can cause mechanical obstruction and the appearance of stridor breathing. This pathology is detected in premature infants with rickets.
Etiological factor

As mentioned above, stridor is a manifestation of a particular disease. The cause of the appearance of pathological noise during breathing can be congenital malformations of the respiratory system, gastrointestinal tract, as well as the cardiovascular system.
Often, stridor develops in acute infectious diseases and disappears after complete recovery. Allergic reactions, accompanied by laryngeal edema, can also manifest as stridor breathing.
Benign and malignant neoplasms of the larynx act more often as a causative factor for stridor in adults. The appearance of a pathological symptom is possible, due to traumatic injury to the larynx or aspiration of a foreign body. And also possible compression of the larynx from the outside, that is, a tumor of the esophagus or inflammation of the thyroid tissue.
Congenital stridor
Congenital stridor occurs immediately after the birth of a child. The leading manifestation is noisy, rough breathing. Congenital pathology may appear later, but this is rare. The mechanism of the occurrence of pathological noises is the same and indicates the appearance of turbulence in air flows passing through the narrow lumen of the larynx.
Causes of congenital stridor
The main causes of congenital stridor are abnormalities in the development of the larynx. Children born prematurely have a softening of the cartilage of the larynx, trachea, bronchi. Such malformations of the respiratory system form mechanical obstacles to the passage of air.
The walls of the respiratory system cannot fully perform their function and bend inward. An insufficient muscular frame of the respiratory system can also contribute to the appearance of a stridor. Less commonly, congenital pathology can be observed with various tumors. The malformations of the respiratory system include choanal atresia, paresis and paralysis of the vocal cords.
Stridor breathing is one of the symptoms of a genetic disorder. This pathology is detected immediately after birth by multiple malformations, phenotypic characteristics, as well as the results of genetic testing.
Manifestations of congenital stridor

Congenital stridor in newborns manifests itself in the first day after birth and then may intensify. The noise that a child experiences when breathing can be different in character and timbre. The sonicity of the noise depends on the original cause of the stridor. It is important to note that the level of pathological sound can vary depending on the environment.
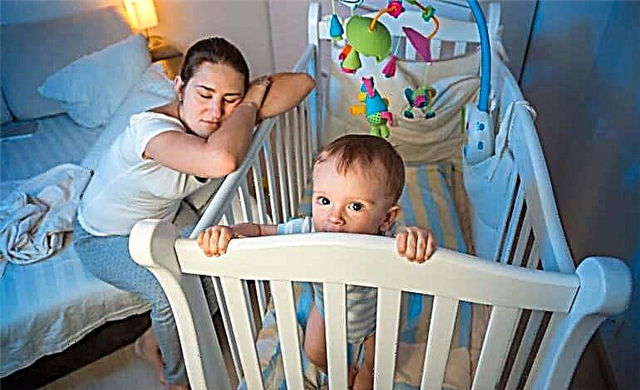
Breathing can be almost silent when sleeping in a warm, moderately humid room. The opposite picture is observed with crying, coughing, sucking and swallowing. The neonatal period often proceeds without features. Children under one year old can gain weight poorly and, therefore, lag behind in physical development, there may also be a violation of swallowing and a change in voice. But it is worth noting that more often the stridor in children is mild and does not affect the development, food intake and sleep of the child.
The situation is more difficult when an infection is attached. The catarrhal symptoms that manifest themselves in the disease provoke an acute attack of stridor. The child's condition worsens, shortness of breath is observed, the skin turns blue when breathing, at the height of inspiration, retraction of the pliable areas of the chest (intercostal spaces, jugular fossa, epigastric region) can be noted. The severe course of the disease can lead to an attack of suffocation, which is a life-threatening condition, often leads to a detailed outcome and requires immediate medical attention. Congenital stridor can cause the development of serious diseases: bronchial asthma, pneumonia, tracheitis and bronchitis.
Treatment approaches
Before starting treatment, it is important to identify the cause of the pathological symptom. In the case of a mild course of stridor, you can take an observational tactic, not forgetting about the constant monitoring of an otorhinolaryngologist. Indeed, after 6 months of life, the situation, as a rule, improves, and by 3 years this symptom disappears completely.
If a child has mechanical obstacles to the air flow in the form of benign tumors, then their surgical removal is indicated. Surgical intervention is also possible for pathology of the cartilaginous skeleton of the respiratory tract. Special attention is required for situations with a layer of infections, then with attacks of stridor, immediate hospitalization is required to prevent a life-threatening condition.
Acquired stridor in children. Causes
Acquired stridor has other causes. In young children, the development of a pathological symptom after aspiration of a foreign body is most characteristic. Today, bronchial asthma in children is quite common. It is the allergic edema of the airways that leads to the appearance of stridor breathing.
Complications after acute tonsillitis - retropharyngeal abscess, epiglottitis act as a mechanical obstacle to the passage of air. An enlarged thyroid gland and tumors of the esophagus, larynx, bronchi or trachea are also causes of stridor development. Cicatricial narrowing of the respiratory gap in the larynx region may occur after prolonged intubation.
Acquired stridor in adults
The causes of acquired stridor in adults are practically the same as in children. But of greater importance are allergic edema and tumors of various organs located near the larynx.
Typical clinical symptoms
The main clinical symptom is a loud breathing noise heard from a distance. By the nature of the noise, you can determine the level of damage to the respiratory tract. As a rule, the volume of the stridor indicates the degree of narrowing of the respiratory gap. The louder the noise, the narrower the gap. But a suddenly abated murmur is often a poor indicator and indicates complete airway obstruction.
It is also important to pay attention to the timbre of the noise. For example, a high stridor frequency indicates a lesion at the level of the vocal cords. A low timbre indicates a lesion above the ligaments, that is, in the region of the upper part of the larynx. Average murmur height shows lesion below the vocal cords.
Specialists identify forms of noise that are also important in finding the cause of this symptom. Inspiratory noise occurs during inspiration and has a low pitch. Expiratory stridor, on the other hand, is observed during expiration and is characterized by an average noise frequency. And the last, biphasic, develops during inhalation and exhalation, has a high pitch.

Examination of children with stridor
Diagnosis of children with this symptom is extremely important, since treatment should be carried out in the direction of the underlying disease. Before the examination, the specialist must carefully collect anamnesis, find out the onset of the appearance of pathological noise, and determine the shape of the stridor. After all, congenital and acquired noise has different causes. It is important to determine the duration and severity of the symptom. The doctor determines what additional symptoms may occur during stridor breathing. In children, it is always important to assess the physical and neuropsychic development, as well as to learn about the features of the perinatal history.
Basic diagnostic methods
- Physical examination. It is necessary to conduct an external examination of the patient and record the existing deviations. On palpation, it is important to identify possible formations in the face and neck. It is important to evaluate other vital signs: breathing rate and depth, heart rate.
- Instrumental diagnostic methods. The "gold standard" in the diagnosis of stridor is fibrorinopharyngolaryngoscopy. This method can be used without the use of general anesthesia, which is certainly an advantage. If necessary, it is possible to use local anesthesia and vasoconstrictor drugs. The instrument is inserted into the nasal cavity and advanced further, assessing all the structural elements of the respiratory system. This method can even be performed on premature babies, since the fiberscope has several sizes. Using this method, you can visually determine the cause of stridor breathing. If necessary, other diagnostic methods may be prescribed, such as X-ray, ultrasound, computed tomography, and magnetic resonance imaging of the larynx. After consulting other specialists, it is possible to assign additional methods.
Differential diagnosis
Differential diagnosis is carried out, first of all, with true and false croup. Also with laryngitis, lymphogranulomatosis, abscesses of retro- and paratonsillar tissue. Fibrorinopharyngolaryngoscopy allows you to make the correct diagnosis with high accuracy.
Stridor treatment
Treatment for stridor breathing depends on the initial cause of the pathological symptom.
Stridor can pass without a trace by 2 - 3 years.
Children with mild stridor should be monitored regularly by a pediatrician, otorhinolaryngologist and pulmonologist. Doctors assess the dynamics of the patient's condition, and as it worsens, remedial measures can be taken. In most cases, in children with stridor, the tactic is expectant.
Drug therapy and its possibilities
Medicines are used when stridor occurs as a result of allergic edema. In this situation, hormonal drugs - glucocorticosteroids (Prednisolone, Pulmicort) can be prescribed. Also, hormone replacement drugs are prescribed for diseases of the thyroid gland.

Surgery
Surgical therapy is also indicated for the treatment of the underlying disease. Surgical intervention is used for aspiration of a foreign body, softening of the cartilage of the larynx, neoplasms in the larynx. In emergency cases, when there is a risk of developing acute respiratory failure, oxygen is prescribed to patients. With complete obstruction of the airways, a tracheotomy (dissection of the tracheal cartilage) is indicated, followed by the placement of an endotracheal tube and artificial ventilation of the lungs.
Forecast
The prognosis in most cases, when the cause of the stridor lies in the anatomical features of the respiratory system, is favorable. And in other situations, the prognosis directly depends on the underlying disease. A more serious situation, which is not excluded a lethal outcome, is observed with the development of acute respiratory failure.
Stridor prevention
A child with this pathological symptom should be constantly monitored by specialists. Parents should create a favorable environment at home, so as not to provoke an increase in pathological noise during breathing. It is important to monitor the psychological state of the child and correct it in time. Up to 3 years old, it is necessary to prevent acute viral and bacterial infections that can cause suffocation in a child.

Conclusion
Stridor is far from a harmless condition that requires careful monitoring by medical professionals. Regular examination of the child allows you to identify and prevent chronic pathology of the respiratory system. Also, constant monitoring of the patient's condition will save him from surgical intervention.