The main causes of intestinal infections in children
Intestinal infection in children is usually caused by viruses, bacteria and their toxins, protozoa or parasites.
Viruses
Viruses are the most common cause of intestinal infections in children. Among them, rotaviruses are the most common culprits in the development of the disease.
In addition, the following viruses are found:
- Noraviruses;
- Astroviruses;
- Reoviruses;
- Enteroviruses (Coxsackie, EKHO);
- Adenoviruses;
- Coronaviruses;
- Orboviruses;
- Toroviruses.
The list of viruses is huge and new pathogens of intestinal infections are constantly being discovered, as well as diagnostic methods are being improved. In recent years, there has been an increase in the number of detected cases among viruses - noraviruses and enteroviruses.

Bacteria
Bacterial intestinal infections are less common than viral infections, but in these cases, complications develop more often.
The list of the most relevant bacterial pathogens at present:
- Salmonella;
- Shigella;
- E. coli (Escherichia coli);
- Staphylococci;
- Cholera vibrio;
- Clostridia;
- Yersinia;
- Campylobacter.
Despite the fact that such a particularly dangerous infection as cholera does not occur in the CIS countries, you should not forget about it in any case, since it exists in some countries. The disease is highly contagious, very severe and can be fatal. This must be borne in mind when planning travel with a child, especially to exotic countries.
Bacterial intestinal infections are dangerous by the development of a formidable complication - hemolytic uremic syndrome.
It is manifested by the development of acute renal failure, hemolytic anemia and thrombocytopenia. The culprit in this situation is usually Shigella, E. coli.
Often, outwardly, the child is active in behavior and the severity of his intestinal symptoms is declining, only a pronounced decrease in urine output is alarming, and urea and creatinine increase in the biochemical blood test. In the general analysis of blood platelets, erythrocytes, hemoglobin are sharply reduced. Such children need long-term treatment in the intensive care unit.

Toxins
An intestinal infection clinic can develop after ingestion of chemical toxins contained, for example, in poisonous mushrooms, spoiled canned food (for example, botulinum toxin), and exotic seafood.
This category of children must be provided with emergency assistance. In this case, the children are admitted to the intensive care unit for further treatment and observation.
In addition, some medications (antibiotics, antipsychotics and others) can cause an intestinal infection clinic in a child.
Other pathogens - Protozoa
These include:
- Cryptosporidium;
- Amoebas;
- Giardia.
Infection routes
The main route of infection with intestinal infections is fecal-oral. This means that a virus or bacteria in the stool (stool) gets into the baby's mouth and causes the disease.
Of course, children do not eat faeces, but their particles with pathogenic pathogens can be in the hands of the parents or the caregiver if they do not wash their hands thoroughly. Also, any object (toys, food, nipple, bottles, etc.), which is touched with dirty hands, becomes infected. Children touch this object with their hands and then pull their hands into their mouth or the object itself, and thus can easily become infected.
The pathogen can enter the body with food or contaminated water. Insufficiently cooked or raw foods (meat, eggs, shellfish and others), unpasteurized milk and juices can be sources of bacterial pathogens.
In addition to the bacteria themselves, food products also contain their toxins, which also provoke the development of the disease. In such cases, they use the term "food poisoning" or, in everyday life, food poisoning.
Do not forget about the dangers of consuming raw water from wells, streams, pools, including water parks.
Animals, both domestic and wild, can carry the disease. These are large and small cattle, chickens, geese, ducks, cats, dogs. Rodents (mice, rats, hamsters) can cause the development of dangerous infectious diseases (for example, yersiniosis).
Infection can occur through contact from other children or adults. Especially in crowded places, in closed groups (schools, kindergartens).
Intestinal infections occur all year round, but there has been a slight increase in their number from November to April.
Classification of intestinal infections (forms of course)
All intestinal infections are subdivided according to the organ principle of damage into the following forms.
- Gastritic - vomiting is the leading symptom. There is no loose stool.
- Gastroenteric - in the clinic there is both vomiting and loose stools. There are no impurities in loose stools.
- Enterocolytic - the leading symptom is loose stools with the presence of pathological impurities in the form of mucus, greenery and blood streaks.
- Enteric - in the clinic, loose stools without pathological impurities (usually watery in nature) prevail.
Symptoms of intestinal infections
The symptoms of intestinal infections are usually similar. It can only be assumed by the clinical symptoms of the disease is viral or bacterial etiology.
Common symptoms
Common symptoms of intestinal infections are vomiting, diarrhea, abdominal pain of varying intensity, and fever. The severity of all these symptoms is different and the severity of the disease directly depends on this. Some symptoms may not be present at all.
In everyday life, you can often find such a name for intestinal infections as "intestinal flu".
All diarrhea is classified as watery (secretory) and invasive. Watery diarrhea is most commonly caused by viral agents. With this variety, the stool gradually loses fecal impurities and becomes like water. Many parents even describe this condition as "the child pissing booty."
Invasive diarrhea is usually caused by bacteria. The stool in this case has impurities of mucus, streaks of blood and greenery. The amount of stool is scant, but its frequency is usually high. It is this group of diarrhea that is threatened by the development of such a complication as hemolytic uremic syndrome (Gasser's syndrome), which was described earlier.
The peak incidence of intestinal infections in children is observed between the ages of 6 months and 2 years.

Some of the most common intestinal infections
Rotavirus infection
Rotavirus infection accounts for 70% of all cases of intestinal infections in children. This is the most common cause of severe childhood diarrhea. An increase in the incidence is observed in the autumn-winter period. Mostly children aged 6 months to 3 years are ill. This age group is also a risk group for the development of severe complications.
The incubation period for this infection is from 24 hours to 7 days (usually within 72 hours). The route of transmission of this infection is fecal-oral or household.
The disease develops acutely and most often occurs in the form of gastroenteritis. At the same time, vomiting, loose stools and fever appear. Vomiting is often repeated, indomitable and is observed on average for 3 days.
Loose stools in typical cases of a watery, foamy character, and in children of the first year of life, admixtures of mucus and blood may be observed. Fluid and electrolyte losses are often significant and lead to the development of severe dehydration. Abdominal pain can be of different intensity and localization. Relief of symptoms of the disease is usually observed within 7 days.
Immunity after the transferred infection is unstable and short-lived.
A vaccine has been developed to prevent rotavirus infection. It is not yet included in the national immunization schedules, but is already available almost everywhere and the CDC recommends it for use primarily in young children.
Noravirus infection
The second most common cause of acute intestinal infections is noravirus infection. Children of school age and adults are more often affected. This infection is characterized by winter seasonality. The incubation period is short and is usually 24-48 hours. The source of infection is a sick person.
In the clinical picture, vomiting comes to the fore. It can be multiple. In addition, there may be abundant loose, watery stools. Symptoms last for 1-3 days. The course of the disease is usually milder than with rotavirus infection.
After the transferred viral intestinal infections, secondary lactase deficiency may develop.
Salmonellosis
Of the bacterial pathogens, one of the most common intestinal infections is salmonellosis. The sources of this infection are usually animals, less often a sick person or a carrier of bacteria. In most cases, the carriers are chickens, geese, pigs, cows, bulls, goats, sheep and others.
Chicken, eggs, pork, beef and unpasteurized milk can contain salmonella from food. Moreover, infection can occur both from infected animal meat, and during the process of cooking, butchering it, as well as storing food.
The rise in the incidence of salmonellosis is noted in the summer-autumn period. The incubation period is 5 to 72 hours. The disease begins acutely and can proceed in the form of various forms, but more often it occurs in the form of a gastroenterocolitic form. That is, the symptoms are represented by vomiting, loose stools with the presence of pathological impurities and fever.
For salmonellosis, the color of the stool is considered to be dark green, the color of "swamp mud". The chair, as a rule, is scarce, but its frequency per day can reach 15 times or more. The duration of intestinal symptoms can be up to 2 weeks, and in children under 1 year old - 1 month. Salmonellosis is dangerous by the development of generalized forms with multiple organ damage.
Children with the presence of immunodeficiency conditions, concomitant chronic pathologies, and young children are at risk for the development of such a severe course. The age peak of the incidence of salmonellosis is observed at the age of 4 years.

Differences in the clinic of intestinal infections in children and adults. What shouldn't be allowed?
Intestinal infections tend to be easier in adults than in children. The relief of symptoms of the disease in adults is observed faster than in children.
Often, in one family, one of the parents gets sick first, and then the child.
Children have less body weight than adults, and the percentage of water in the body is much higher. In newborns, it reaches 85%. For an adult, this figure is 65%. Therefore, children are much more susceptible to the development of dehydration and shock. Moreover, this can happen in a short period of time. The risk group for the development of dangerous complications is made up of children in the first year of life. Therefore, it is very important to give children water to drink in order to prevent the development of such serious complications.
What is needed to confirm the diagnosis?
Diagnoses "Acute intestinal infection", "Acute gastroenteritis", "Acute enterocolitis", etc. - these are primarily clinical diagnoses. That is, the doctor exposes them after receiving anamnesis data and examining the patient. There are a great many causative agents of intestinal infections, but laboratory tests are carried out only to detect the most common in practice.
In addition, the sensitivity and specificity of diagnostic methods are less than 100%. The most specific diagnostic methods are expensive and are not available in all medical institutions, and more often the identification of a specific pathogen does not change anything in the treatment of the child.
Therefore, in some cases, one can find in the discharge epicrisis such a formulation of the diagnosis as "Diarrhea and gastroenteritis of presumably infectious origin."
History and physical findings
In the anamnesis, the doctor specifies a recent contact with a patient with gastroenteritis, the use of poor-quality or insufficiently heat-treated food or raw water, a violation of the rules of personal hygiene.
Traveling to other countries is important, as the frequency of occurrence of pathogens varies from country to country. Some pathogens are currently found only in a limited list of countries.
It is important to identify recent contact with animals, including pets. Also, if you, for example, live in a private house with a cellar, then you should not forget that rodents like to live in such places, which are carriers of various infections.
During the examination, the doctor must pay attention to the child's behavior, whether he has signs of dehydration. In addition, differential diagnosis with acute surgical pathology in the presence of severe abdominal pain is always carried out.
With intestinal infections, increased intestinal peristalsis is observed, abdominal pain can be diffuse, in the epigastric, left iliac regions. The doctor must check with the parents the amount of diuresis and the amount of fluid consumed for the current day.

Laboratory diagnostics to help the doctor
From laboratory diagnostics, bacteriological and serological methods are used. Pathogens are detected in the stool or blood of the child.
The bacteriological method consists in sowing feces or blood on special media. The method is informative, but it takes a long time to get the results.
From serological methods, enzyme-linked immunosorbent assay (ELISA), passive hemagglutination reaction (RPHA), complement fixation reaction and others are used. The sensitivity of the methods is high, but the disadvantage is that most of them cannot be used in the early stages of the disease.
The polymerase chain reaction (PCR) method is highly sensitive, fast in obtaining the result and informative in the early stages. But the method is expensive and not available everywhere.
In addition, general clinical analyzes are also used. A complete blood count for intestinal infections is nonspecific. With bacterial infections, leukocytosis may occur with a shift in the formula to the left. However, with viral infections in the first 2 days of the disease, the same picture can be observed.
In the biochemical analysis of blood with the bacterial nature of the disease, an increase in C-reactive protein is noted.
On ultrasound of the abdominal organs, enlarged mesenteric lymph nodes are often found.

Therapeutic tactics
Treatment of intestinal infections depends on the severity of the disease and the nature of the pathogen.
When can the child be left at home?
The child can be left at home if he is active. If he can drink, eat, and most importantly, absorb it. If he does not have pronounced signs of dehydration. If the child does not have a decrease in the number and volume of urination.
Hospital referral
Most often, young children, especially the first year of life, get to the hospital. This is due to the fact that the percentage of water in their body is much higher than that of an adult and is 80-85%.
Dangerous signs of dehydration in a child are as follows:
- dry lips and visible mucous membranes;
- a large fontanelle on the head of infants sinks (below the level of the bones of the skull);
- the amount of excreted urine is reduced and its color is saturated;
- the child is lethargic, sleepy;
- in very severe cases - when the child is crying, then there are no tears, eyes are sunken, the skin fold on the body straightens slowly (longer than 3 seconds), there is no thirst.
In these cases, the treatment of the child must necessarily be carried out in a hospital setting.
The main stages of treatment and drugs
In most cases, the treatment of intestinal infections is symptomatic.
Etiotropic treatment
Etiotropic treatment is prescribed only in the case of a bacterial nature of the disease in the form of antibacterial drugs. The choice of the drug is carried out taking into account the alleged pathogen, the possibility of oral administration of drugs.
For example, with salmonellosis - Amoxicillin, Trimethoprim-sulfamethoxazole, Azithromycin in age-related dosages. If it is impossible to take an antibiotic inside, moderate and severe forms, with a generalized version, intravenous antibacterial drugs are prescribed (cephalosporins of 3-4 generations (Ceftriaxone, Cefotaxime), aminoglycosides (Amikacin), carbapenems (Meropenem).
With viral etiology, no antiviral drugs are prescribed. Antibacterial drugs in these cases not only do not help, but can also harm the child.
Sorbents
Prescription of enterosorbent preparations is a mandatory component in the treatment of any intestinal infection. They help control symptoms. In age dosages, Smectite, Enterosgel, Activated carbon, Polysorb, Polyphepan and others are used. They are given before the child has relieved the symptoms.

Rehydration therapy
Watering the child is mandatory for all intestinal infections.
Drinking is carried out with ready-made glucose-salt solutions (Normohydron, Oralit, Gastrolit and others), potassium compote from dried fruits, sweet tea without flavors. The child needs to be given liquid fractionally, that is, 1-2 teaspoons every 5 minutes. This process always requires the patience and perseverance of the parents. For young children, it is convenient to use a syringe without a needle, a pipette, a bottle with a nipple.
With the ineffectiveness of drinking and the development of dehydration in the child, it is necessary to carry out infusion therapy with glucose-salt solutions in a hospital setting.
Antiemetic drugs
Antiemetic drugs are indicated only in cases of persistent and indomitable vomiting in a child and should be used with caution. This group of drugs, if used unreasonably for intestinal infections, can aggravate the child's condition.
From antiemetic drugs, Motillium (Motillac), Ondansetron can be prescribed. These drugs should not be given to a child without a doctor's prescription.
The antidiarrheal drug Loperamide (Imodium) is contraindicated for all intestinal infections and can cause serious complications! It paralyzes the intestinal motility and there is a massive accumulation of toxins and pathogens in the intestinal lumen.
Caring for a child after stopping acute manifestations of intestinal infection
After the relief of acute manifestations of intestinal infection, specific child care is usually not required. Gradually, the child's usual daily routine should be restored.
Diet
The diet should also be thermally and mechanically gentle.
In children under 1 year of age, breastfeeding should be continued. If the child is bottle-fed, then it is preferable to use low-lactose or lactose-free formulas.
It is necessary to exclude from the diet foods rich in coarse fiber, carminative (cabbage, legumes), whole milk. It is preferable to use boiled, steamed dishes.

Mode
The regimen during the period of fever and active intestinal manifestations should be bed or semi-bed. After the relief of the main symptoms, the regimen gradually approaches the usual for the child.
Do you need additional medications?
If residual manifestations persist or in the case of the development of bacterial carriers, courses of probiotics can be recommended.
Taking probiotics during the acute period can shorten the duration of diarrhea by an average of 2 days. Of the large number of drugs presented in the pharmacy network, only drugs containing Sacchoromyces boulardii and Lactobacillus GG have an evidence base for effectiveness. But if they are prescribed, then they should be applied in a course of at least 3-4 weeks.
With the development of enzymatic (disaccharidase) deficiency, as a rule, the appointment of enzyme preparations is not required. In this case, it is enough to adhere to an elimination diet (exclude foods containing lactose).
Possible complications and prognosis of the disease
With timely treatment, the prognosis for intestinal infections is favorable. The relief of symptoms of the disease in most cases is observed within 3-7 days.
However, in case of untimely and inadequate treatment, the presence of concomitant severe pathology and in early childhood, the following complications of the disease may develop:
- the development of dehydration (dehydration) up to hypovolemic shock;
- electrolyte imbalance (hypokalemia, hyponatremia, hypernatremia);
- lactase deficiency;
- hemolytic uremic syndrome;
- susceptibility to reinfection;
- intolerance to cow's milk;
- multiple organ failure;
- death.
Prevention of intestinal infections in children
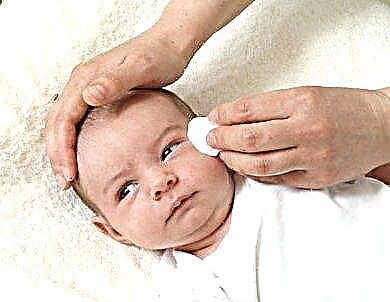
The main thing in the prevention of intestinal infections is adherence to the rules of personal hygiene in adults caring for children. It is also necessary to ensure that the child does not pull dirty hands, toys, etc. into his mouth.
- It is imperative to develop personal hygiene skills in your child.
- Wet cleaning should be carried out regularly in the apartment, especially the places where diapers are changed for the child.
- It is imperative to use only well thermally processed meat products and only pasteurized milk.
- Observe the storage conditions for products and do not use them if these conditions are violated.
- Raw water from open sources should not be consumed.
- Be sure to wash your hands with soap and water after dealing with animals.
- Treat work surfaces after cooking. You should use different dishes and utensils for raw and prepared foods.
- Be sure to wash raw vegetables and fruits thoroughly before consuming them.
- If there is a person in the family with symptoms of vomiting or diarrhea, then his contact with the child should be limited.

Conclusion
The problem of the development of intestinal infections and their treatment in children remains relevant throughout the world. Remember that the best way to prevent intestinal infections is to teach children to wash their hands and not consume contaminated water and food that has been stored in a way that has not been stored properly.