In recent decades, unfortunately, this disease is gaining strength among children and adolescents. Juvenile chronic arthritis in children (JCA) is an autoimmune disease. Infection is believed to be one of the suspected causes.
Per 100 thousand of the child population, JUHA falls ill from 2 to 16 children.
Arthritis is also may be:
- vaccination (more often after DPT);
- joint injury;
- hypothermia;
- excessive insolation (sun exposure);
- hereditary predisposition.
Juvenile rheumatoid arthritis is more common in girls.
Joint anatomy
 To understand the essence and classification of JUHA, let's figure out what the joint consists of.
To understand the essence and classification of JUHA, let's figure out what the joint consists of.
A joint is a connection of the bones of the skeleton, immersed in the joint capsule, or bursa. Thanks to them, a person can show any physical activity.
The bursa consists of an outer and an inner layer. The inner layer or synovium is a kind of nourishment for the joint.
In children, the joints are abundantly supplied with the vasculature.
With JHA, inflammation occurs in the synovial membrane, hence the trophism (nutrition through the blood supply) of the joint and further changes are disturbed.
Juvenile arthritis in children and its classification
By the number of affected joints arthritis is subdivided into:
- monoarthritis - one joint is affected;
- oligoarthritis - when no more than four joints are involved;
- systemic variant - damage to organs and tissues joins the damage to the joints;
- polyarthritis - more than four joints are damaged.
By detection of rheumatoid factor in the patient's blood:
- seropositive;
- seronegative.
For the development of complications:
- infectious complications;
- macrophage activation syndrome;
- articular pain syndrome in a child;
- pulmonary heart failure;
- growth retardation.
Painful articular syndrome in a child
 Pain is the most basic complaint in children with rheumatoid arthritis, so if arthritis is suspected, the mother should pay attention to the following factors:
Pain is the most basic complaint in children with rheumatoid arthritis, so if arthritis is suspected, the mother should pay attention to the following factors:
- redness and swelling of the joint;
- the skin over the joint is hot to the touch;
- the child spares the joint, limiting movement in it;
- pain when flexing, extending the affected limb;
- in the morning, stiffness in the joint, that is, the inability to get out of bed or brush your teeth on your own due to limited mobility in the joint.
Juvenile rheumatoid arthritis, seropositive
The prevalence is about 10%. They are more often affected by girls aged 8 - 15 years.
Joint pain occurs symmetrically. Knee, wrist and ankle joints are more often affected.
This type is not the best option for the course of the disease, since it leads to destructive (destructive) changes in the joint in the first six months of the disease. The child has impaired flexion / extension of the joint with subsequent disability.
Complications:
- growth retardation;
- severe disability;
- contractures (lack of mobility) in the joints.
Such a severe course and complications are associated with the presence of rheumatoid factor in the blood, which is quite aggressive to the synovial membrane of the joint and leads to irreversible consequences without adequate treatment.
Juvenile arthritis, seronegative
Distributed in 20 - 30%. Again, the female sex from 1 to 15 years old suffers more often, the age range is wider than that of the seronegative.
The course of this disease is benign.
Joints are affected:
- knee;
- elbow;
- temporomandibular joints;
- cervical spine.
Also, with this form of JHA, mothers may notice in the child an increase in temperature and an increase in lymph nodes.
Comparison table
| Seronegative | Seropositive |
|---|---|
| Affects children from a year | More often children 8-15 years old are sick |
| In 10% of cases, it is complicated by destruction | More often destructive processes or joint destruction develop |
| The course is more benign. There may be inflammatory eye changes as a complication | Ankylosis develops rapidly - disorders of mobility in the joints of the wrist, ankles |
| The joints are affected symmetrically, that is, equally on the right and on the left. |
Oligoarthritis
It occurs in 50% of all cases.
Several joints are affected:
- Knee.
- Ankles.
- Elbow.
- Wrist.
The course of this form of the disease is quite aggressive, as inflammatory changes develop in the membranes of the eye.
Systemic variant of rheumatoid arthritis
Clinical manifestations:
- rash;
- enlargement of the liver, spleen;
- temperature rise;
- joint pain;
- inflammatory changes in organs.
Complications of the disease
1. Eye damage. Children with juvenile arthritis may experience inflammatory changes in the membranes of the eye.
 As a rule, this happens asymptomatically, and the child does not feel pain in the eyes at all, which is fraught with the threat of loss of vision without proper control of the ophthalmologist.
As a rule, this happens asymptomatically, and the child does not feel pain in the eyes at all, which is fraught with the threat of loss of vision without proper control of the ophthalmologist.
With juvenile arthritis, iritis or iridocyclitis, inflammation of the iris of the eye, often occurs.
Complications of eye diseases:
- cataract - clouding of the lens;
- glaucoma - increased intraocular pressure;
- as the most unfavorable outcome - blindness.
Your attending rheumatologist is obliged to refer your child to an ophthalmologist for a check-up twice a year.
The oculist should only use a slit lamp to examine these babies. Without it, the inspection will be incorrect. As a consequence, the doctor may miss the problem with the eyes in juvenile arthritis.
If the doctor detects the onset of inflammatory changes in the eye, treatment will be prescribed. They will treat with eye drops, which are based on a hormonal component to reduce dryness, swelling and inflammation.
If, after a course of treatment with eye drops, the positive effect does not occur, then it is necessary to reconsider the treatment of juvenile rheumatoid arthritis, prescribe stronger drugs.
Also, eye treatment is possible by introducing an injection drug into the eyeball. This significantly increases the effectiveness of the treatment of the underlying disease.
2. Damage to organs and systems.Juvenile rheumatoid arthritis is a disease that affects not only the joints, but also the internal organs. The disease affects the connective tissue, which is present in many organs, and the blood vessels.
Major targets for arthritis:
- Heart.
- Lungs.
- Kidneys.
- Nervous system.
Inflammatory changes in the lining of the heart are called carditis. They can also develop as complications after other diseases. For example, after suffering streptococcal sore throat or scarlet fever, which are more characterized by damage to the cardiac valve system. With juvenile arthritis, changes in the myocardium and pericardium often occur. Carditis can be asymptomatic.
Changes in the lungs concern the lung tissue itself and the pleura. The bronchi and bronchioles themselves suffer less often. As complications in the pleural cavity, adhesions occur and fluid accumulates.
Pain in the arms and legs is a consequence of rheumatic damage to the nerve endings. Movement disorders can also occur.
Kidney damage occurs in the form of glomerulonephritis (inflammation of the kidney tissue). Moreover, glomerulonephritis occurs when arthritis is highly active. Kidney failure does not occur, usually minimal changes in urine appear.
Diagnostics
1. If your child begins to complain of joint pain, then immediately follow the pediatric cardio rheumatologist or pediatric rheumatologist.
 2. At the initial stage of examinations, the child should be passed:
2. At the initial stage of examinations, the child should be passed:
- general blood analysis;
- general urine analysis;
- biochemical blood test (liver enzymes, creatinine, total protein, blood sugar, C - reactive protein);
- blood for the presence of rheumatoid factor;
- blood for the study of the titer of antistreptolysin O (if there is a history of frequent tonsillitis), which indicates the presence of streptococcus in the body;
- blood test for immunological parameters (antinuclear factor, circulating immune complexes, concentration of immunoglobulins).
3. Then the doctor will direct the baby to instrumental examinations:
- Ultrasound of the affected joints;
- X-ray examination;
- Ultrasound of the abdominal cavity;
- ECG;
- Ultrasound of the heart (with suspected carditis);
- Ultrasound of the kidneys.
4. Professional consultation. An optometrist, an ENT doctor, a neurologist must examine the child if there are complaints.
Only after the examinations passed above, the doctor must confirm or deny the diagnosis.
Regime moments in treatment
- With active arthritis, bed rest or significant limitation of physical activity is indicated. Jumping, running, squatting are prohibited.
JUHA is always treated in a hospital setting.
- Minimal dosed exercises for the joints are required. Joints are made to move. Gymnastics should be carried out with an exercise therapy instructor. An individual approach to each child is important, taking into account his functional abilities and pain.
- With juvenile arthritis, you should not use plaster cast, apply splints, bandages on the affected joint.
- Mandatory medical removal from vaccinations.
- Exclusion of hypothermia.
- Sun exposure is only permitted with sunscreen and hats.
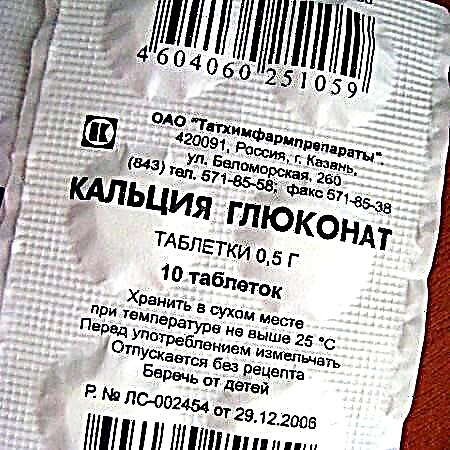
- A diet enriched with calcium is recommended, complete with balanced meals.
- Psychological support and the right attitude on the part of the parents, since the treatment of JUHA can last for years.
Essential medicines for treatment
In this matter, it should be noted two directions of treatment:
- Symptomatic treatment. These are non-steroidal anti-inflammatory drugs and glucocorticosteroids.
- Immunosuppressive therapy that suppresses the activity of the immune system.
Non-steroidal anti-inflammatory drugs (NSAIDs)
 These drugs relieve pain quite well, but not so well eliminate inflammatory changes in juvenile arthritis.
These drugs relieve pain quite well, but not so well eliminate inflammatory changes in juvenile arthritis.
These include:
- Nise;
- Ibuprofen;
- Diclofenac;
- Meloxicam.
In rheumatology, Nise, or Nimesulide, is often and widely used. It has been proven that of all non-steroids, it has the mildest effect on the child's body and has fewer side effects.
Anti-inflammatory drugs of a hormonal nature
In the presence of systemic arthritis with organ damage, the so-called pulse therapy is prescribed.
Pulse therapy is an intravenous infusion of hormonal drugs (Prednisolone) in high enough doses. Not recommended for children under 3 years of age, as it may cause stunted growth.
Immunosuppressants
Hormonal drugs have a quick but short-term effect.
Therefore, with ineffectiveness and high activity of the disease, as well as with the systemic variant, immunosuppressants are prescribed.
Methotrexate is the main drug used to treat rheumatoid arthritis. Immunosuppressive therapy should be long-term, in age-related dosages, without spontaneous withdrawal.
Quite often it happens that, against the background of treatment with methotrexate, the child develops remission, all symptoms go away and the parents decide to cancel the drug without the consent of the doctor. As a result, a sharp exacerbation of the disease occurs and, possibly, with a more aggressive course.
Cancellation of methotrexate is carried out only in a hospital setting and, at least, after a 2-year remission.
Methotrexate is quite effective and is well tolerated in most cases. Nausea, vomiting is possible, but this is at the initial stage of treatment.
The dosage of Methotrexate is selected in a hospital setting, calculated by weight, height. It happens both in tablet form and injectable, it is taken once every 1 - 2 weeks as prescribed by a doctor.
JUHA is a disease in which a child must be assigned a disabled status. This entitles you to free medication. But, unfortunately, the commission does not always award disability to such children, therefore, they have to be treated at their own expense.
New in treatment
 More recently, for the treatment of juvenile arthritis, drugs - biological agents:
More recently, for the treatment of juvenile arthritis, drugs - biological agents:
- Aktemra;
- Humira;
- Orencia;
- Remicade.
These drugs are proteins that bind to and suppress immune cells. Treatment with these drugs is expensive and is not carried out in all clinics.
1 ampoule of such a drug can cost up to 70,000 rubles. Such treatment is possible at the expense of the MHIF budget.
How to achieve long-term remission?
Remission is considered:
- lack of joints with active arthritis;
- lack of systemic manifestations;
- normal blood and urine counts, negative C-reactive protein and rheumatoid factor;
- complete absence of complaints from the child;
- morning stiffness no more than 15 minutes.
If within six months the child passes these criteria, then we can safely talk about remission.
In general, arthritis treatment is a complex and, most importantly, a long process. It can take years. Of course, the child's quality of life suffers. An important role in this is played by how the immune system responds to treatment, whether the dosage is correctly selected, whether the patient receives it.
Juvenile rheumatoid arthritis can only be cured through the well-coordinated work of the doctor and parents.