In children's medical practice, there are very dangerous conditions that require special treatment. One of these pathologies is pyloric stenosis.
What it is?
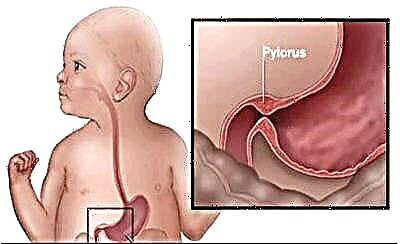
A pathological condition in which the pylorus of the stomach is significantly narrowed is called pyloric stenosis. This pathology is most often congenital. Boys, according to statistics, get sick more often than girls. The first adverse symptoms of a congenital form of the disease appear already in newborn babies.
Pyloric stenosis can also be acquired. Typically, these clinical forms of the disease occur in older children. Most often this is a consequence of a severe form of gastric ulcer or a consequence of a chemical burn of the inner gastric wall. Congenital forms of the disease are found in children's practice much more often than acquired ones. Conservative treatment in these situations is completely ineffective.

Currently, scientists have not established a single cause that causes the development of narrowing of the pylorus of the stomach. They identify several causal factors that most often contribute to the development of the disease. These include:
- Various viral infections that the child suffered during intrauterine development.
- Complicated pregnancy. Severe toxicosis, especially in the late stages of gestation, contributes to various disorders of organogenesis in the baby. After birth, the child develops various anatomical defects in the structure of internal organs, as well as functional disorders, often manifested by pylorospasm.
- Long-term use of certain medicines.
- Expressed endocrinological diseases in the expectant mother.
Various intrauterine pathologies lead to the appearance of clinical signs of pyloric stenosis in a child after birth. Normally, the pylorus of the stomach ensures the normal passage of the food bolus through the digestive tract. This function is called evacuation. If food does not leave the stomach and stagnates in it for a long time, then this ultimately leads to overstretching of its walls.
Violation of food evacuation contributes to the appearance of specific clinical manifestations in the baby.
Symptoms
In the development of the disease, several stages are successively replaced: compensation, subcompensation and decompensation. If the diagnosis of gastric pathology was carried out untimely or treatment was too delayed, then the extreme stage - decompensation - is quickly reached. The nature of this disease is programmed. Over time, the severity of symptoms only increases.
The initial stage of the disease in young children is not yet accompanied by the development of adverse symptoms. Usually at this time the child is practically not worried about anything. In some cases, the symptoms can be minimal, which does not cause any concern for the general condition of the baby from the parents. The disease is detected, as a rule, at a rather late stage.
The first symptom in infants, which should alert parents, doctors consider the appearance of a feeling of overflow in the epigastric region. After a while, the baby starts to vomit the food eaten. Pieces of food in this case remain practically undigested.
This is an important diagnostic criterion for vomiting, which occurs precisely with pyloric spasm.

As the disease progresses vomiting occurs after almost every meal. Even eating a little, the child feels strong gagging. After vomiting, the baby feels much easier. In the later stages of the disease, a child has a vomiting urge even after drinking liquids: compote, fruit drink, tea, juice and even plain water. Such pronounced vomiting leads to the fact that the baby loses much weight. In the child's body, pronounced electrolyte and metabolic disorders appear.
Prolonged stagnation of food in the stomach leads to increased putrefactive and fermentative processes in it. As a result of this, the baby develops or worsens chronic diseases of the gastrointestinal tract. Almost all babies with a long course of pyloric stenosis develop persistent chronic gastritis with impaired gastric secretion.
Disruption of food intake into the intestines leads to problems with the absorption of various nutrients, as well as vitamins from food. This contributes to the fact that the baby is significantly behind in physical development from their peers. Sick children do not gain weight well, and in some cases even lose weight a lot. Babies usually lag behind not only in physical, but also in mental development.
This feature is due to the need for optimal intake of nutrients and vitamins in early childhood every day.


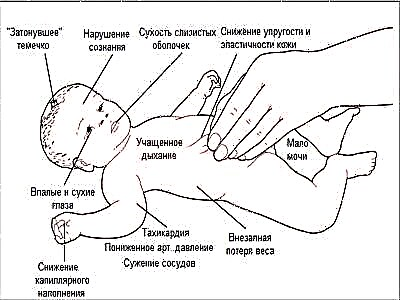
Severe vomiting contributes to the development of many symptoms of dehydration in the baby. The baby's skin becomes very dry. The severe course of the disease contributes to the appearance of a characteristic appearance: the face is stretched, the nose is sharpened, the cheekbones are clearly delineated. The skin becomes pale, blue small veins are clearly visible on it. Visible mucous membranes turn pale, and an intolerable feeling of dryness appears in the mouth.
Severe and frequent vomiting contributes to the baby often asks for a drink. In severe stages of the disease, this does not improve well-being, since drinking fluids only contributes to more frequent vomiting.
In severely weakened and slender babies, stomach peristalsis and overflow become visible.
The lack of intake of necessary nutrients in the body leads to the fact that the baby constantly feels a growing feeling of hunger. A high appetite persists for a long time in the child and only progresses with the development of the disease. Increasing vomiting leads to the fact that the baby has severe constipation. Overflow of the stomach contributes to the occurrence of pain in the epigastric region.
Diagnostics
When the first clinical symptoms of the disease appear, it is very important to urgently consult a doctor. The doctor will conduct a full clinical examination and examination of the baby, which is necessary for the correct diagnosis. During the examination, the doctor must palpate the abdomen and determine the size of the organs of the gastrointestinal tract.
The specialist will also be able to identify overflow in the stomach and assess the severity of other functional pathological conditions.
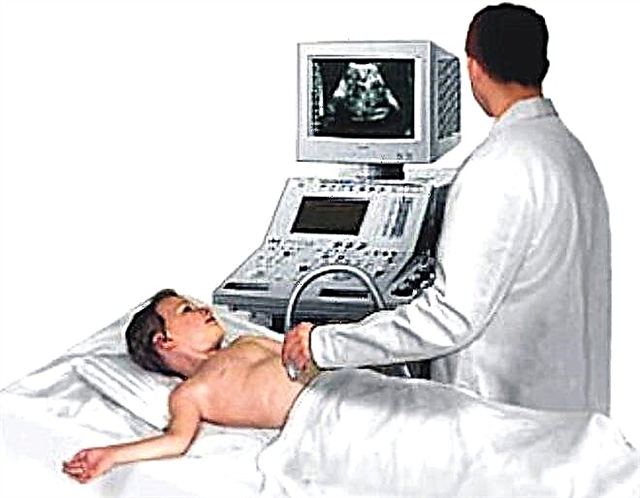
To establish metabolic disorders, the doctor will prescribe a mandatory blood test for the child. You can examine the organs of the gastrointestinal tract using an ultrasound examination. Another, more unpleasant examination, is an endoscopic examination of the upper digestive system. With the help of special devices - endoscopes, doctors examine all anatomical parts of the stomach, and also determine the presence and volume of stagnant contents in it.
In the late stages of the disease, endoscopic examination reveals signs of cicatricial narrowing. They can also be present in babies with acquired forms of pyloric stenosis resulting from chemical burns of the gastric mucosa with various substances. For older children, in order to exclude the narrowing of the gatekeeper, radiography. It also helps to establish the severity of the existing anatomical defects.


Currently, gastric x-rays in children are used less and less. This method has been replaced by various ultrasound examinations, which make it possible to more accurately and reliably clarify the presence of existing narrowings in the stomach. Ultrasound does not carry radiation exposure, like radiography, which means it can be used even in the smallest patients.
In diagnostics, it is very important to distinguish organic (structural) defects from functional ones. Pyloric stenosis is an organic pathology characterized by the presence of a pronounced narrowing in the pylorus. Pylorospasm is a functional disorder associated with a violation of the nervous innervation of an organ. In some cases, to conduct a differential diagnosis between these two pathological conditions, doctors resort to prescribing antispasmodic course regimens.
Usually, the use of these funds leads to an improvement in well-being in pyloric spasm and practically does not have a persistent therapeutic effect in pyloric stenosis.
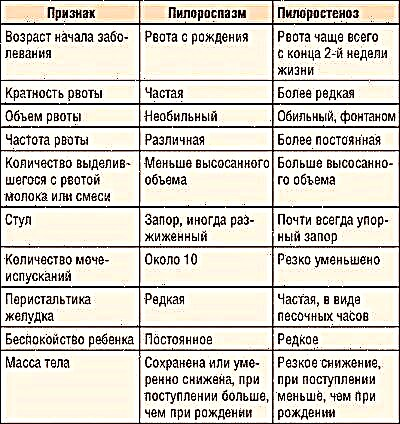
What is the difference between pylorospasm and pyloric stenosis, see the following video.
Treatment
To eliminate the adverse symptoms of the disease, various types of surgical treatment are performed. The choice of the operation is carried out by the pediatric surgeon, taking into account the initial state of the child, his age and the presence of concomitant chronic diseases in the child. Most often, surgical treatment of pyloric stenosis is performed routinely.
In pediatric surgical practice, it is often used the Frede-Ramstedt operation. This method is as gentle as possible for the delicate organism of the child. During the operation, surgeons perform a layer-by-layer dissection of the mucous and muscular membranes, reaching the gatekeeper. During surgical treatment, there is no effect on the mucous membrane. This gentle technique can significantly reduce the likelihood of postoperative complications.
Having reached the narrowed section of the gatekeeper, the doctors carry out sequential opening of a dense muscle ring. This contributes to the fact that the mucous membrane can straighten out on its own without making surgical incisions on it. Subsequently, the size of the stomach gradually returns to normal, and all unfavorable clinical symptoms of pyloric stenosis completely disappear.
During surgery, doctors also work with the nerves that provide the innervation to the stomach. This contributes to the consolidation of the positive effect of the performed surgical treatment.
Even a severe course of pyloric stenosis is an indication for surgery. If the surgical treatment is not performed on time, the child rapidly develops dangerous complications. In some cases, it can even be fatal. Pyloric stenosis is a rather dangerous clinical condition that requires urgent treatment.