Cystic fibrosis in children is a chronic, progressive and often fatal genetic (hereditary) disease. Cystic fibrosis primarily affects the respiratory and digestive systems. The sweat glands and the reproductive system are also affected.
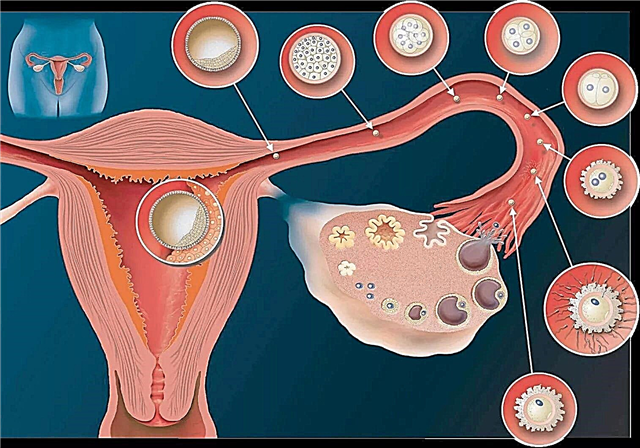
Genetic causes
Cystic fibrosis in children is caused by a faulty gene that controls the body's absorption of salt. In case of illness, too much salt and not enough water enter the cells of the body.
 This turns the fluids that normally "lubricate" our organs into thick, sticky mucus. This mucus blocks the airways in the lungs and clogs the lumen of the digestive glands.
This turns the fluids that normally "lubricate" our organs into thick, sticky mucus. This mucus blocks the airways in the lungs and clogs the lumen of the digestive glands.
The main risk factor for developing cystic fibrosis is family history, especially if either parent is a carrier. The gene that causes cystic fibrosis is recessive.
This means that in order to have this disease, children must inherit two copies of the gene, one from mom and dad. When a child inherits only one copy, he does not develop cystic fibrosis. But this baby will still be a carrier and can pass the gene on to its offspring.
Parents carrying the cystic fibrosis gene are often healthy and asymptomatic, but will pass the gene on to their children.
In fact, according to various estimates, up to 10 million people may be carriers of the cystic fibrosis gene and not know about it. If mom and dad have a defective gene for cystic fibrosis, then they have a 1: 4 probability of having a child with cystic fibrosis.
Symptoms
Signs of cystic fibrosis are manifold, and they can change over time. Usually, symptoms in children first appear at a very early age, but sometimes they show up a little later.
Although this disease causes a number of serious health problems, it mainly affects the lungs and the digestive system. Therefore, the pulmonary and intestinal form of the disease is allocated.
Modern diagnostic methods can detect cystic fibrosis in newborns using special screening tests before any symptoms appear.
- 15 - 20% of newborns with cystic fibrosis have meconium obstruction at birth. This means that their small intestine is clogged with meconium, the original stool. Normally, meconium leaves without any problem. But in babies with cystic fibrosis, it is so dense and dense that the intestines simply cannot remove it. As a result, the bowel loops twist or do not develop properly. Meconium can also block the colon, and in this situation, the baby will not have a bowel movement for a day or two after birth.
- Parents themselves may notice some of the signs of cystic fibrosis in newborns. For example, when mom and dad kiss a baby, they notice that his skin tastes salty.
- The child is not gaining enough body weight.
- Jaundice can be another early sign of cystic fibrosis, but this symptom is not reliable, as many babies develop this condition immediately after birth and usually resolves after a few days on their own or with the help of phototherapy. It is more likely that the jaundice in this case is associated with genetic factors, and not with cystic fibrosis. Screening allows doctors to make an accurate diagnosis.
- The sticky mucus produced by this disease can cause serious damage to the lungs. Children with cystic fibrosis often develop chest infections because this thick fluid forms a fertile ground for bacteria to grow. Any child with this condition suffers from a series of severe coughs and bronchial infections. Severe wheezing and shortness of breath are additional problems that babies suffer from.
While these health problems are not unique to children with cystic fibrosis and can be treated with antibiotics, the long-term consequences are serious. After all, cystic fibrosis can cause such damage to a child's lungs that they cannot function properly.
- Some children with cystic fibrosis develop polyps in their nasal passages. Babies may have severe acute or chronic sinusitis.
- The digestive system is another area where cystic fibrosis becomes the main cause of damage. Just as sticky mucus blocks the lungs, it also causes comparable problems in different parts of the gastrointestinal system. This interferes with the smooth passage of food through the intestines and the system's ability to digest nutrients. As a result, parents may notice that their child is not gaining weight or growing normally. The baby's stool smells bad and looks shiny due to poor digestion of fats. Children (usually over four years old) sometimes suffer from intussusception. When this happens, one part of the intestine is inserted into another. The intestine folds telescopically into itself, like a television antenna.
- The pancreas is also affected. Often inflammation develops in it. This condition is known as pancreatitis.
- Frequent coughing or difficult stools sometimes cause rectal prolapse. This means that a portion of the rectum protrudes or exits the anus. About 20% of children with cystic fibrosis experience this condition. In some cases, rectal prolapse is the first noticeable sign of cystic fibrosis.
Thus, if a child has cystic fibrosis, he may have the following manifestations and symptoms, which can be both mild and severe:
 cough or wheezing;
cough or wheezing;- the presence of a large amount of mucus in the lungs;
- frequent lung infections such as pneumonia and bronchitis;
- shortness of breath;
- salty skin;
- slow growth, even with good appetite;
- meconium obstruction in newborns;
- Frequent stools that are loose, large, or fatty
- stomach pain or bloating.
Diagnostics
When symptoms begin to appear, cystic fibrosis is not, in most cases, the doctor's first diagnosis. There are many symptoms of cystic fibrosis, and not every child has all of the symptoms.
Another factor is that the disease can vary from mild to severe in different children. The age at which symptoms appear also changes. Some were diagnosed with cystic fibrosis in infancy, while others were diagnosed later in life. If the disease is mild, the child may not have problems until adolescence or even adulthood.
Genetic examination
By passing genetic tests during pregnancy, parents can now find out if their future children may have cystic fibrosis. But even when genetic tests confirm the presence of cystic fibrosis, there is still no way to predict in advance whether a particular child's symptoms will be severe or mild.

Genetic testing can also be done after the baby is born. Since cystic fibrosis is a hereditary condition, the doctor may suggest testing the baby's siblings, even if they have no symptoms. Other family members, especially cousins, should also be tested.
A baby is usually tested for cystic fibrosis if the baby is born with meconium ileus.
Sweat sample
After birth, the standard diagnostic test for cystic fibrosis is the sweat test. It is an accurate, safe and painless diagnostic method. The study uses a small electric current to stimulate the sweat glands with pilocarpine. This stimulates the production of sweat. Within 30-60 minutes, sweat is collected on filter paper or gauze and checked for chloride levels.
A child must have a sweat chloride test of over 60 on two separate sweat samples to be diagnosed with cystic fibrosis. Normal sweat values for babies are lower.
Determination of trypsinogen
The test may not be informative in newborns, as they do not produce enough sweat. In this case, another type of test can be used, such as the determination of immunoreactive trypsinogen. In this test, blood taken 2 to 3 days after birth is analyzed for a specific protein called trypsinogen. Positive results should be confirmed by sweat test and other tests. In addition, a small percentage of children with cystic fibrosis have normal sweat chloride levels. They can only be diagnosed by chemical tests for the presence of the mutated gene.
Other types of examination
Some of the other tests that can help diagnose cystic fibrosis are chest x-rays, lung function tests, and sputum analysis. They show how well the lungs, pancreas, and liver are working. This helps determine the extent and severity of cystic fibrosis once it is diagnosed.
These tests include:
 chest x-ray;
chest x-ray;- blood tests to assess the amount of nutrients entering the body;
- bacterial studies that confirm the growth of Pseudomonas aeruginosa and Staphylococcus aureus or other hemophilic bacteria in the lungs. These bacteria are widespread in cystic fibrosis, but may not affect healthy people;
- pulmonary function tests to measure the effect of cystic fibrosis on respiration.
Pulmonary function tests are performed when the child is old enough to collaborate in the testing process;
- stool analysis. It will help identify gastrointestinal abnormalities that are characteristic of cystic fibrosis.
Treatment of cystic fibrosis in children
- Since cystic fibrosis is a genetic disease, the only way to prevent or cure it is to use genetic engineering at an early age. Ideally, gene therapy can repair or replace a defective gene. At this stage in the development of science, this method remains unrealistic.
- Another treatment option is to give the child with cystic fibrosis an active form of a protein product that is either insufficient or not in the body. Unfortunately, this is also not feasible.
So at present, neither gene therapy nor any other radical treatment for cystic fibrosis is known to medicine, although drug-based approaches are now being studied.
In the meantime, the best doctors can do is to ease the symptoms of cystic fibrosis or slow the progression of the disease to improve the child's quality of life. This is accomplished with antibiotic therapy combined with procedures to remove thick mucus from the lungs.
The therapy is tailored to the needs of each child. For children whose disease is very progressive, lung transplantation may be an alternative.
Previously, cystic fibrosis was a fatal disease. Better therapies developed over the past 20 years have increased the average lifespan of people with cystic fibrosis to 30 years.
Lung disease treatment
The most important area of treatment for cystic fibrosis is the fight against shortness of breath, which causes frequent lung infections. Physiotherapy, exercise, and medication are used to relieve mucosal blockages in the airways of the lung.
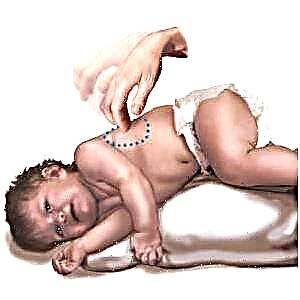 bronchial (postural) drainage. It is carried out by placing the patient in a position that allows mucus to drain from the lungs, that is, the level of the shoulders is below the level of the lower back. During the procedure, the chest or back is clapped and vibrated to activate the mucus and help it out of the airways. This process is repeated in different areas of the chest to reduce the amount of mucus in different areas of each lung. This procedure should be performed every day. And it is very important to teach this technique to family members;
bronchial (postural) drainage. It is carried out by placing the patient in a position that allows mucus to drain from the lungs, that is, the level of the shoulders is below the level of the lower back. During the procedure, the chest or back is clapped and vibrated to activate the mucus and help it out of the airways. This process is repeated in different areas of the chest to reduce the amount of mucus in different areas of each lung. This procedure should be performed every day. And it is very important to teach this technique to family members;- Exercise helps flush mucus and stimulate coughing to clear the lungs. It can also improve the overall physical condition of the child;
- of medicines, aerosol medicines are used to facilitate breathing.
These medications include:
- bronchodilators that widen the airways;
- mucolytics that thin mucus;
- decongestants that reduce swelling in the airways
- antibiotics to fight lung infections. They can be given orally, in an aerosol form, or injected into a vein.
Treating digestive problems
Digestive problems in cystic fibrosis are less severe and easier to control than lung problems.
A balanced, high-calorie diet is often prescribed that is low in fat and high in protein and pancreatic enzymes that aid digestion.
Vitamin A, D, E, and K supplements are indicated for good nutrition. Enemas and mucolytics are used to treat intestinal obstruction.
Caring for an infant with cystic fibrosis
When you are told that your baby has cystic fibrosis, you need to take extra steps to make sure the newborn is getting the nutrients it needs and that the airway remains clear and healthy.
Feeding
To aid proper digestion, you will need to give your baby the enzyme supplements prescribed by your doctor at the beginning of each feed.
Since young children often eat, you should always carry enzymes and baby food with you.

Signs that your child may need enzymes or an enzyme dose adjustment include:
- inability to gain weight despite a strong appetite;
- frequent, greasy, foul-smelling stools;
- bloating or gas.
Children with cystic fibrosis need more calories than other children in their age group. The amount of extra calories they need will differ depending on the lung function of each infant, the level of physical activity and the severity of the disease.
A child's caloric requirements may be even higher during illness. Even a mild infection can significantly increase calorie intake.
Cystic fibrosis also disrupts the normal function of the cells that make up the sweat glands of the skin. As a result, babies lose large amounts of salt when they sweat, leading to a high risk of dehydration. Any additional salt intake should be dosed as recommended by a specialist.
Education and development
The child can be expected to develop according to the norm. When a toddler enters kindergarten or school, he or she can receive an Individualized Education Plan under the Persons with Disabilities Education Act.
An individualized plan ensures that your child can continue their education if they fall ill or go to the hospital, and also includes the necessary arrangements for visiting an educational institution (for example, providing additional time for snacks).
Many children with cystic fibrosis continue to enjoy childhood and grow up leading fulfilling lives. As a child grows up, he may need a lot of medical procedures and occasionally go to the hospital.
The child should be encouraged to be as active as possible. Your little one may need extra help from a parent to adjust to school and everyday life.The transition from childhood to adulthood can also be challenging as the child must learn to manage cystic fibrosis on their own.
Above all, children with cystic fibrosis and their families must maintain a positive attitude. Scientists continue to make significant strides in understanding the genetic and physiological abnormalities in cystic fibrosis and in developing new treatment approaches such as gene therapy. There is a prospect for further improving the care of patients with cystic fibrosis and even for the discovery of a treatment!

 cough or wheezing;
cough or wheezing; chest x-ray;
chest x-ray;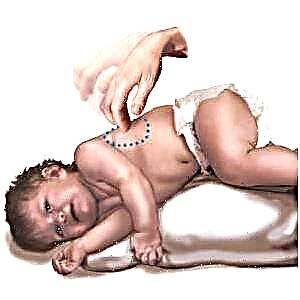 bronchial (postural) drainage. It is carried out by placing the patient in a position that allows mucus to drain from the lungs, that is, the level of the shoulders is below the level of the lower back. During the procedure, the chest or back is clapped and vibrated to activate the mucus and help it out of the airways. This process is repeated in different areas of the chest to reduce the amount of mucus in different areas of each lung. This procedure should be performed every day. And it is very important to teach this technique to family members;
bronchial (postural) drainage. It is carried out by placing the patient in a position that allows mucus to drain from the lungs, that is, the level of the shoulders is below the level of the lower back. During the procedure, the chest or back is clapped and vibrated to activate the mucus and help it out of the airways. This process is repeated in different areas of the chest to reduce the amount of mucus in different areas of each lung. This procedure should be performed every day. And it is very important to teach this technique to family members;