It is simply impossible to determine how the fetus grows and develops without performing a number of studies. Screening of the 2nd trimester of pregnancy is a very important medical method for such a diagnosis.
What it is?
Screening doctors call a whole set of examinations, which is necessary in order to identify various developmental anomalies in the fetus, and also to determine how well it develops in the mother's womb. Pregnancy is a unique period in the life of every woman. At this time, the hormonal background changes significantly. This causes the basal hormone levels to change. Also, specific biochemical markers may appear in the blood, which indicate the possible development of genetic and chromosomal pathologies.
In each of the periods of bearing a baby, pathologies manifest themselves in different ways. They can be determined only by the method of laboratory diagnostics and ultrasound. Such studies are prescribed by an obstetrician-gynecologist. The expectant mother learns about screening, usually at the very first visits to the women's clinic. Screening during pregnancy is a recommendation procedure. Not all women decide to pass it.
Quite often, only expectant mothers who have any concomitant diseases of internal organs undergo prenatal screening.
The introduction of prenatal screening in our country happened relatively recently. The frightening demographic situation led to the development of such recommendations of doctors. Doctors note that the introduction of prenatal screening has significantly reduced maternal mortality rates. Thanks to this diagnostic complex, doctors began to identify dangerous genetic abnormalities at the earliest stages of their formation.

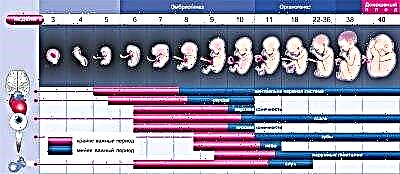
The second trimester is the period when the embryo has passed to the next stage of its development. At this time, doctors already determine the future baby as a fetus. The child continues to undergo differentiation of all vital systems of the body. This time is no less important than the first trimester of pregnancy. A full-fledged second screening includes a set of general clinical and biochemical analyzes, hormonal studies, and is also complemented by the mandatory ultrasound scan. In some cases, doctors may slightly expand the list of required tests.
Quite often this happens in a situation where the expectant mother was found to have some abnormalities during the screening of the 1st trimester of pregnancy.

Many mothers believe that screening can prevent congenital genetic diseases from developing in their babies. It should be noted right away that, unfortunately, this is not the case. It is possible to prevent the appearance of chromosomal pathologies in a baby at the stage of preparation for pregnancy..
If conception has already occurred, then it is no longer possible to influence the formation of a specific genetic disease. However, it is possible to identify certain pathologies with the help of screening quite often. Such dangerous diseases as Down's disease, Edwards syndrome, Patau's syndrome and many other diseases can be determined using a specific set of diagnostics, which is carried out in the 2nd trimester of pregnancy. Also, screening allows you to determine various malformations and anomalies in the structure of tubular bones.
Quite often, these tests also reveal congenital metabolic diseases, such dangerous pathologies include galactosemia, phenylketonuria, cystic fibrosis and many others.
Dates
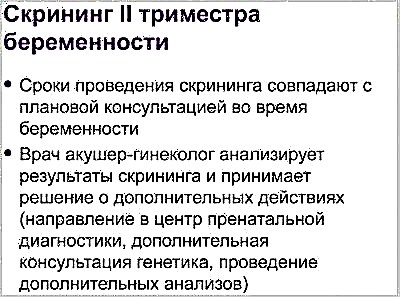
Doctors have established several decreed periods of pregnancy, in which screening is most rational. In each of the trimesters of bearing a baby, there is one such complex of diagnostics. The timing is determined for all women. There are also certain clinical situations where they can be slightly shifted.

In this case, the specific dates of the screening are determined by the obstetrician-gynecologist observing the patient.
In most situations, a complex of studies is carried out at 16-20 weeks of pregnancy. As an exception, screening can be done after 21 weeks. Usually this situation occurs when a pregnant woman has any neoplasms in the ovaries. With these pathologies, the hormonal background changes significantly. To obtain more accurate results of biochemical analyzes, the screening is postponed by 1-2 weeks.

Many mothers believe that an ultrasound scan should be done on the same day with a trip to the laboratory. This is not necessary at all.
It may even take several weeks between the blood tests and the ultrasound examination, this situation is quite normal.
Who should be screened for?
Obstetricians-gynecologists recommend passing such a complex to all women carrying babies, however, there are certain groups that just need screening. Women who have indications for a study should not skip the complex of prenatal diagnostics. This can lead to the fact that doctors simply do not find out in a timely manner about the presence of dangerous pathological conditions in the future mother and her baby. Doctors identify several decreed categories of women who simply need to be screened.
These groups include the following:
- Future mothers who conceived a baby after 35 years;
- Pregnant women with congenital malformations or a burdened family history of genetic or chromosomal diseases;
- Expectant mothers who have deviations from the norm in the tests or by ultrasound during the 1st pregnancy screening;
- Pregnant women suffering from severe diseases of internal organs;
- Expectant mothers with a burdened course of the 1st trimester of pregnancy with frequent threats of spontaneous miscarriage;
- Pregnant women who are forced to take immunosuppressive or hormonal medications for medical reasons while carrying a baby.


If doctors reveal dangerous pathologies of fetal development in the future mother during the 1st screening or later on ultrasound, then in this case she is sent for additional diagnostics to the perinatal center. There, more experienced doctors perform expert-level ultrasound examinations.
In some situations, pregnant women with certain medical conditions are screened only in such perinatal centers.


Training
To get reliable and accurate results, it is very important for the expectant mother to prepare correctly. A few days before the delivery of biochemical tests, she should definitely follow a lipid-lowering diet. It implies restriction of all fatty and fried foods in the daily diet. Fast food, smoked meats and pickled dishes are also completely excluded. Dinner on the eve of the study should be light. It is optimal if it consists of a protein dish, supplemented with a side dish of any cereal. Vegetables and fruits should be limited before an ultrasound scan, they can lead to increased gas formation, and the presence of gas in the abdomen will not allow the ultrasound doctor to see the fetus and all membranes well.

Also, 2-3 days before the ultrasound examination, legumes and all types of cabbage are necessarily excluded. Drinking kvass or carbonated drinks also significantly increases gas production. It is better that, on the eve of the planned tests and ultrasound, all food is as light as possible, but nutritious.
It is very important for a pregnant woman to eat enough protein, even before laboratory tests.

Exercise can also lead to inaccurate results. Doctors have long noticed that simply climbing stairs can cause changes in biochemical parameters. For, for the results of laboratory tests to be accurate, the expectant mother should limit all physical activity... In this case, cleaning the apartment or visiting yoga for pregnant women should be postponed for a few days after the screening.
Biochemical tests should be done necessarily on an empty stomach... Some experts allow expectant mothers to drink some water before testing. You should not eat breakfast before going to the laboratory.
Testing should be done in the morning. Studies carried out in the evening give less truthful results.


Currently, doctors recommend that mothers-to-be should limit all highly allergenic foods before taking biochemical tests. This is due to the fact that every day there is more and more scientific research that suggests that such food can affect the receipt of reliable results.
For a week before being tested for screening for the 2nd trimester, it is better to exclude all citrus fruits, seafood, chocolate and honey from your menu.

Analysis standards
Biochemical screening of the 2nd trimester is of very important diagnostic value. The results of the blood tests obtained are not yet a diagnosis at all, they only help doctors navigate the possible pathologies of the course of pregnancy and anomalies in the development of the fetus at this stage of its intrauterine development. HCG is an important laboratory marker that can reveal certain "hidden" pathological conditions. Its dynamics change throughout pregnancy. In the first weeks of intrauterine development of the fetus, the concentration of this hormone in the blood is maximum. Then, over time, it begins to decline.
Before childbirth, the concentration of hCG in the blood drops rapidly.
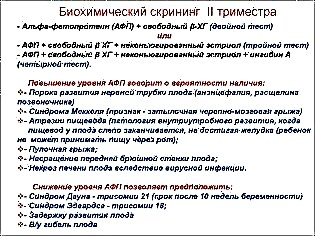
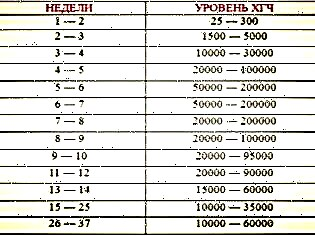
At 16 weeks of gestation, normal hCG blood levels reach 4.7-50 ng / ml. By week 20, this value already rises above 5.3 ng / ml. Quite often, an increase in hCG occurs with multiple pregnancies. A significant excess of this indicator may indicate the possible development of Down's disease or Edwards syndrome.
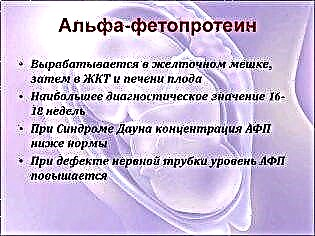
Alpha-fetoprotein is another specific pregnancy hormone that is used to assess the intrauterine development of an unborn baby. It is formed by the gastrointestinal tract and the liver of the fetus. By the end of 10-11 weeks, it begins to flow through the general uteroplacental system of blood flow and into the mother's body. Normal values of this indicator at 16-19 weeks of pregnancy are 15-95 units / ml.
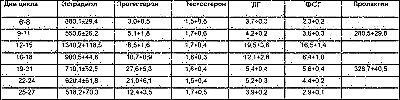
Free estradiol is the third indicator that shows how well a particular pregnancy is going. To a greater extent, it reflects the functional ability of the placenta. The normal course of pregnancy is accompanied by a gradual increase in this hormone in the blood of the expectant mother. By week 16, the values of this hormone are 1.17-5.5 ng / ml.
To assess the risk of various chromosomal pathologies, more and more often, doctors prescribe non-invasive hemotest to expectant mothers. It allows you to identify the DNA of the fetus and assess the presence of any genetic diseases. Significant disadvantages of this study are the possibility of conducting it only in the largest Russian cities and the high cost.
Such studies are prescribed only for strict genetic medical indications.


Interpretation of ultrasound results
The second trimester of pregnancy is the time when it is already possible to determine not only the outline of the fetus's body, but also to evaluate the work of its internal organs. For this, doctors have developed a number of special indicators. They help doctors conduct a more comprehensive assessment. Future mothers should remember that the conclusion of an ultrasound scan is not a diagnosis. It only describes all the visual changes that the specialist saw during this study.

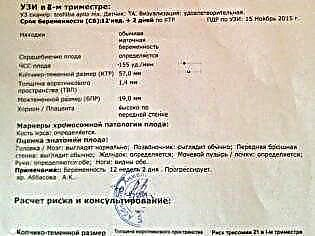
Fetometry is one of the methods of ultrasound diagnostics, with the help of which the doctor determines the size of the main anatomical elements of the fetus. During the study, the doctor takes measurements of the head, shoulders, limbs of the future baby. His presentation is also necessarily determined. However, it should be noted that quite often babies begin to move actively in the third trimester of pregnancy. This contributes to the fact that the presentation can change.

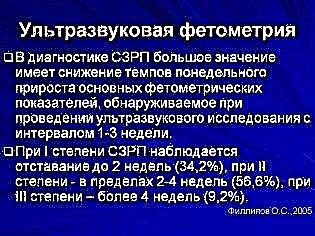
To assess the normal development of a child's skeleton, doctors use the following indicators:
- Biparietal size of the fetal head... At 16 weeks, it is 26-37 mm, and by 20 weeks it changes to 39-56 mm.
- Frontal-occipital size... At 16 weeks, its values are 32-49 mm, at 20 weeks they change to 53-75 mm.
- Femur length... At 16 weeks of gestation, the indicator values are 13-23 mm. By week 20, they increase to 23-38 mm.
- Chest diameter... At 16 weeks of gestation, normal values for the indicator are 11-21 mm. By week 20, they increase to 21-34 mm.
- Humerus length... At 16 weeks of gestation, normal values for the indicator are 13-23 mm. By week 20, they increase to 24-36mm.
- Chest circumference... At 16 weeks of gestation, normal values of the indicator are 112-136 mm. By week 20, they increase to 154-186 mm.
- Abdominal circumference... At 16 weeks of gestation, normal values for the indicator are 88-116 mm. By week 20, they increase to 124-164 mm.


The next step in assessing the development of the fetus is to determine the anatomy of its internal organs. For this, the specialist determines the boundaries and parameters of the liver, stomach, intestines, heart, gall bladder. At this time of development of the fetus, it is already possible to assess its heartbeat. This indicator is also quite important for assessing intrauterine development.
It is very important to evaluate the parameters of the fetal brain at 2 ultrasound screening. The normal size of the cerebellum at week 16 is 12-15 mm... By the end of week 20, it is already 18-22 mm. Also, during the study, an ultrasound specialist assesses the size of the lateral ventricles and cisterns. The values of these indicators at this stage of the baby's development are 10-11 mm.

The membranes are very important anatomical structures. They protect the fetus from the effects of various external factors. In the 2nd trimester, the amniotic fluid index is determined, this indicator is also called the amniotic fluid index. It helps doctors assess whether a pregnant woman has oligohydramnios.

Normally, at the 16th week of pregnancy, the amniotic fluid index should be 73-201 mm.
You can find out in more detail about what the 2nd trimester screening includes by watching the following video.