Your child wakes up in the middle of the night agitated, has nausea and a stomach ache, then vomits. Typically, these symptoms are as little as 24-hour indigestion. But sometimes there is another reason. Symptoms of pancreatitis in children are often similar to those of rotavirus, which is confusing to many parents.
Children's pancreatitis usually resolves quickly without long-term damage to the pancreas. It is important to recognize symptoms early to reduce the risk of complications. The baby may need treatment or nutritional changes for a short time.
What is infantile pancreatitis?
 Pancreatitis is an inflammatory disease of the pancreas. The pancreas is an organ that is part of the digestive system and is located anatomically just behind the stomach.
Pancreatitis is an inflammatory disease of the pancreas. The pancreas is an organ that is part of the digestive system and is located anatomically just behind the stomach.
This body produces the hormones insulin and glucagon, which regulate the amount of sugar in the body.
But the pancreas also plays a crucial role in digestion. It produces essential enzymes that help us metabolize the food we eat.
If the pancreas is healthy, the enzymes don't become active until they reach the duodenum. But when the gland becomes inflamed, enzymes are activated at an early stage, while they are still in the organ itself, and aggressively affect the internal structures.
The tissues in the pancreas that produce enzymes are damaged and stop producing new enzymes. Over time, this tissue damage can become chronic.
Causes of pancreatitis in children:
- cholelithiasis. 10% to 30% of children with pancreatitis may have gallstones. Treatment for this condition can help restore normal pancreatic function;
- polyorganic diseases. Twenty percent of cases of acute pancreatitis are caused by conditions affecting multiple organs or organ systems, such as sepsis, hemolytic uremic syndrome, or systemic lupus erythematosus;
- metabolic diseases. Metabolic disorders can be the cause of 2 - 7% of cases of acute pancreatitis. This is a metabolic disorder in children with high levels of lipids or calcium in the blood:
- infections. Acute pancreatitis is sometimes diagnosed when a child is suffering from an infection. However, it is difficult to establish a direct link between these two conditions. Some of the infectious diseases that have been associated with pancreatitis include mumps, rubella, cytomegalovirus, human immunodeficiency virus, adenovirus, and group B coxsackie virus;
- anatomical abnormalities. Disorders in the structure of the pancreas or biliary tract can lead to pancreatitis;
- pancreatitis can be triggered by medication. Drugs are thought to cause one quarter of pancreatitis cases. It is not entirely clear why certain drugs can cause pancreatitis. One factor is that children treated with these drugs have additional disorders or conditions that predispose them to pancreatitis;
- pancreatitis is sometimes caused by trauma. Injury to the pancreas can cause acute pancreatitis. Mechanical damage can occur in a car accident, during sports, when falling or due to abuse of children;
- pancreatitis is hereditary, which means it was passed on by one or both parents. This is due to cystic fibrosis, a genetic mutation that is found in the child but not in the parents;
- finally, there are a large number of cases of pancreatitis where the cause is unknown. This is called idiopathic pancreatitis.
Forms of pancreatitis
Acute pancreatitis
The acute form of pancreatitis is a sharp inflammation that lasts for a short period of time. The course of the disease - from mild discomfort to severe, life-threatening illness. Most children with acute illness recover completely after receiving the right therapy. In severe cases, the acute form leads to organ bleeding, severe tissue damage, infection and cyst formation. Severe pancreatitis damages other vital organs (heart, lungs, kidneys).
In rare cases, repeated attacks of acute pancreatitis will lead to chronic disease, which over time will cause permanent damage to the pancreas.
Symptoms
Acute pancreatitis in children usually goes away quickly, within a week. But it is important to see the symptoms in advance and see a specialist to reduce the risk of complications.

The most common symptom of acute pancreatitis is intense upper abdominal pain. This pain is usually much more severe than typical colic. It can be constant, spasmodic, and worse after eating. At the same time, it is difficult for a child to be in an upright position.
Other signs of pancreatitis in children:
- bloated, tender belly;
- pain radiates to the back;
- nausea;
- vomiting;
- loss of appetite;
- heat;
- cardiopalmus.
The symptoms of pancreatitis are non-specific and can easily be confused with signs of another pathology. They differ depending on the age and developmental level of the child. For example, babies who cannot speak will cry a lot.
Diagnostics
Making a diagnosis is often a challenge. Sometimes pancreatitis is misdiagnosed as constipation, irritable bowel syndrome.
For diagnosis, the doctor will conduct a thorough clinical examination and study the child's medical history.
Specialist will recommend doing:
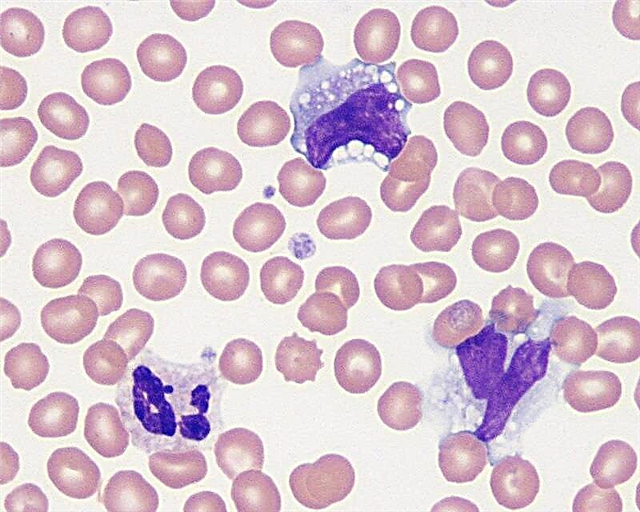
- a blood test to find out how the pancreas is working
- ultrasound procedure;
- computed tomography to check for signs of damage to the pancreas;
- MRI (magnetic resonance imaging) to check for abnormalities in the development of the pancreas
- endoscopic retrograde cholangiopancreatography to examine the small intestine, pancreatic duct, and the rest of the gastrointestinal tract;
- genetic tests to look for a possible hereditary cause.
Treatment of acute pancreatitis in children
Treatment for pancreatitis in children is supportive care. There is no single medicine or treatment to help the pancreas heal. A pain reliever may be given to children with abdominal pain. Nausea and vomiting are treated with antiemetic drugs.
 If the child cannot eat because he has pain, nausea, or vomiting, he is not fed, but fluid is given through a vein to prevent dehydration.
If the child cannot eat because he has pain, nausea, or vomiting, he is not fed, but fluid is given through a vein to prevent dehydration.
The baby can start eating when he feels hungry and is ready to eat. The nutrition plan proposes a specific ration from starter diets ranging from clear nutrient broths to regular foods.
The choice depends on the severity of the child's condition and the preference of the attending physician. The baby, as a rule, regains good health in the first day or two after an attack of acute pancreatitis.
It happens that the symptoms are more severe or persist for a longer period of time. In this case, the baby will be given tube feeding to prevent digestive upset and improve recovery.
Chronic pancreatitis
Chronic pancreatitis in children is also an inflammation of the pancreas. Only instead of the damage that eventually goes away with acute pancreatitis, the inflammation in some more susceptible children continues and causes permanent disturbances in the structure and function of the pancreas. Genetic and environmental factors may be responsible for susceptibility to pancreatitis.
The condition of the disease persists for a long time and slowly destroys the structures of the pancreas. For example, she may lose the ability to produce insulin. As a result, the child develops intolerance to glucose. Chronic pancreatitis also leads to weight loss due to poor digestion.
Chronic pancreatitis is rare in children. The diagnosis can be made in a child of any age, but is more common after 10 years.
Symptoms:
- children usually experience signs and symptoms that are identical to those caused by acute pancreatitis. It is a piercing pain in the abdomen, worse after eating, which will repeat over and over again;
- weight loss is another common symptom. Part of the reason is that the baby is unable to eat. In some cases, children avoid food because it aggravates painful symptoms. Sometimes pancreatitis can cause a decrease in appetite, resulting in weight loss.
Other symptoms of the chronic form of the disease include:
- nausea;
- vomiting (vomiting may be yellowish, greenish or brownish due to an admixture of bile);
- diarrhea and fatty stools;
- digestion disorders;
- yellow skin color;
- there is pain in the back or in the left shoulder.
Diagnostics
Laboratory diagnosis of chronic pancreatitis for a child is similar to acute pancreatitis. The diagnosis of chronic pancreatitis requires looking for permanent damage to the pancreas, loss of digestive function, or diabetes. Damage is assessed using x-rays (CT or MRI scans of the pancreas) and special endoscopic procedures.
Chronic pancreatitis treatment
The clinical guidelines focus on reducing pain and improving digestive function. Damage to the pancreas cannot be repaired, but with proper care, most symptoms can be managed.
You can treat children's pancreatitis in three ways:
Drug therapy
- Pain relievers.
- Digestive enzyme preparations (if enzyme levels are too low) for normal food digestion.
- Fat-soluble vitamins A, D, E and K, as the difficulty in absorbing fat also interferes with the body's ability to absorb these vitamins, which play a crucial role in maintaining health.
- Insulin (with the development of diabetes).
- Steroids, if a child has pancreatitis of autoimmune genesis, which occurs when immune cells attack their own pancreas.
Endoscopic therapy. In some cases, an endoscope is used to relieve pain and remove mechanical obstacles. An endoscope is a long, flexible tube that your doctor puts through your mouth.

This allows the doctor to remove stones in the pancreatic ducts, place small tubes (stents) to strengthen their walls, improve bile flow, or neutralize digestive fluid leaks.
Surgery... Most children don't need surgery. However, if the child has severe pain that does not respond to medication, removing a portion of the pancreas sometimes helps. Surgery is also used to unblock the pancreatic canal or widen it if it is very narrow.
Not all children who experience acute attacks of pancreatitis develop chronic pancreatitis.
There is no clear evidence that a special infant formula is required for chronic pancreatitis. However, many doctors prescribe a low-fat diet and advise patients to eat more often in smaller meals, with less than 10 grams of fat.
Chronic pancreatitis cannot be cured, it is a lifelong condition, symptoms periodically appear and then disappear. Children need to see a doctor regularly to assess their condition, ensure adequate nutrition, and discuss treatment options. He will regularly conduct endocrine studies to identify any problems related to glucose tolerance or the development of diabetes.
Children with chronic illness have an increased risk of pancreatic cancer. The severity level depends on the underlying cause of pancreatitis, family history, and type of genetic involvement.
Reactive pancreatitis in children
Reactive pancreatitis in a child is slightly different from other forms of the disease.
Reactive pancreatitis in children is not an independent disease. This is the response of the child's body to various adverse effects in the form of inflammation of the pancreas.
The causes of this form of the disease:
- Common childhood infectious diseases (ARVI, tonsillitis, etc.).
- Digestive system pathology.
- Abdominal trauma.
- The use of potent antibiotics.
- Poisoning with chemical toxins.
- Irregular eating.
- Products of poor quality and various kinds of "snacks" that are not useful for the child's body.
- Introduction of foods that are not suitable for age (sour juice, meat) into complementary foods for an infant.
Difference between reactive pancreatitis and acute disease:
- Reactive pancreatitis is caused by diseases of other organs, and acute pancreatitis occurs due to direct toxic and damaging effects of various conditions.
- Reactive pancreatitis, if left untreated, becomes acute, but acute pancreatitis will not become reactive.
- Provided the underlying disease is excluded, reactive pancreatitis is effectively treated.
- When determining the symptoms of reactive pancreatitis, the symptoms of the underlying disease are in the foreground, and then the signs of pancreatitis. In acute pancreatitis, the main symptoms are signs of a violation of the pancreas.
- When diagnosing reactive pancreatitis, together with the establishment of symptoms of pancreatitis, symptoms of a disease of other organs are found. And with an acute form - not necessarily.
Similarities:
- Diagnostics is carried out using the same research methods.
- Treatment is prescribed in the same way as in the acute form of the disease.
- Prevention methods often overlap.
Signs of a reactive form of inflammation of the gland can be divided into two groups: clinical manifestations of the underlying disease and signs of pancreatic inflammation itself.
For example, if reactive pancreatitis is triggered by an intestinal infection, there is often a high fever and loose stools several times a day.
The onset is usually acute.
The most common symptoms of reactive pancreatitis
 Severe abdominal pain. The baby is likely to curl up into a fetal position to relieve itself. After the first 2 days, the pain usually gets worse.
Severe abdominal pain. The baby is likely to curl up into a fetal position to relieve itself. After the first 2 days, the pain usually gets worse.
Other signs include:
- persistent vomiting, worse after the first 2 days;
- lack of appetite;
- jaundice (yellow discoloration of the skin);
- high fever;
- back pain and pain in the left shoulder.
Long-term signs include dehydration and low blood pressure.
In small children, the symptoms are smoothed and not very pronounced. The combination of one of these symptoms with persistent abdominal pain is the reason for an immediate appointment with a specialist. Independent attempts by parents to cope with the situation will lead to dire consequences.
Diagnostics:
- When a doctor suspects reactive pancreatitis, the first step is to have blood tests (test for amylase and lipase) to find out if the enzymes in the pancreas are at normal levels.
- If they are too high, the doctor will refer you for an abdominal ultrasound to look for possible signs of inflammation, blockages, or stones in the pancreatic duct.
- Sometimes your doctor will recommend an abdominal CT scan to confirm the diagnosis of pancreatitis.
Treatment
Reactive pancreatitis in children should only be treated in a hospital. Bed rest is required.
Treatment of the reactive form consists of three parts - diet therapy, treatment of the underlying disease, treatment of pancreatitis. Complete recovery of the pancreas is impossible without them.
Diet for reactive pancreatitis in children is of great importance for treatment. For 1 - 2 days (at the discretion of the doctor) food is absolutely excluded in order to provide unloading for the inflamed organ. During this time, the child should be provided with only drink. The amount of water required is determined by the doctor.
The menu is expanding very slowly. The calorie content of food should be small (small portions every 3 to 4 hours). The first two weeks the food is pureed.
Diet for pancreatitis in children
Diet recommendations for pancreatitis:
- a low-fat diet must be followed. Eat fats and oils sparingly;
- eliminate fried foods;
- you can bake food, cook, steam;
- include fruits and vegetables;
- eat often, in small portions.
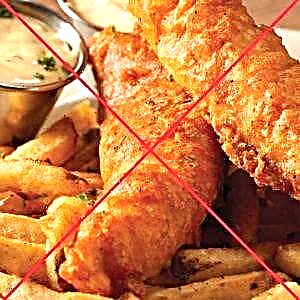 Products that it is necessary to exclude:
Products that it is necessary to exclude:
- fried food;
- semi-finished meat products;
- egg yolk;
- fatty red meat;
- cow's milk;
- butter;
- sour cream;
- margarine;
- ice cream;
- fried beans;
- peanuts and butter from it;
- nuts and seeds;
- corn or potato chips;
- biscuit and shortcrust pastries (muffins, cookies);
- salad dressing (mayonnaise, vegetable oil);
- fat.
What can you eat?
The following foods and dishes should be included in the children's diet:
- low-fat meat dishes;
- a bird without skin;
- egg white;
- low-fat or low-fat dairy products;
- almond, rice milk;
- lentils;
- beans;
- soy products;
- 2nd grade flour bread;
- whole grains;
- rice;
- pasta;
- vegetables and fruits, fresh or frozen;
- vegetable and fruit juices;
- tea;
- vegetable soups;
- water.
The dietary menu for children with pancreatitis should contain foods that have digestive enzymes. For example, pineapples, papaya.
Sample menu
Breakfast:
- two egg whites with spinach;
- One slice of whole wheat toast
- tea.
Lunch:
- an Apple;
- herbal tea.
Dinner:
- rice, red or black beans;
- one flat cake;
- 100 g of chicken breast meat;
- water or juice.
Afternoon snack:
- low-grade flour crackers;
- banana;
- water.
Dinner:
- shrimp pasta;
- a small portion of green salad (no oil) with fat-free sauce or balsamic vinegar;
- juice or water.
Afternoon snack:
- low-fat Greek yogurt with blueberries and honey;
- water or herbal tea.
Talk to your child's doctor and nutritionist about your child's diet. If you have diabetes, celiac disease, lactose intolerance, or other health problems, dietary changes are required.