
More recently, it was generally accepted that gastritis is an occupational disease for adults who are unable to eat full-fledged hot food during the day. Taxi drivers, salesmen, managers of various levels were treated for this ailment. However, today gastritis is rapidly "getting younger", and already 5-6 year old children - and even newborns - are ill with it. You will learn about why gastritis develops in children, how to recognize it, what are the symptoms and treatment, by reading this article.

About the disease
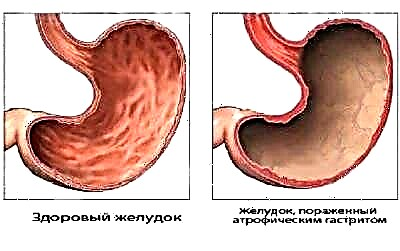
Gastritis is a common ailment of the digestive system, in which the gastric mucosa undergoes inflammatory changes. Moreover, the changes are sometimes dystrophic. The disease develops and lasts for quite a long time, without manifesting itself in any way.

As a rule, by the time the disease is detected, the mucous membranes are already beginning to break down - the normal glands are replaced by fibrous tissue, and the epithelial cells that make up the stomach lining completely atrophy. As a result, the stomach ceases to perform part of its functions (secretory), and this has unpleasant consequences.
With gastritis, a vigorous immune process occurs in the body. When any bacteria or representatives of other species enter the stomach, which the gastric juice cannot cope with on its own, the ubiquitous immunity takes over. He begins with all his might to try to restore the integrity of the membranes of the stomach, strikes at harmful enemies, as a result of which inflammation starts. This process takes a long time, gradually completely changing the composition and functions of the gastric inner membrane.

In a disease that is not caused by immune interference, the mucous membranes are affected by some aggressive external factors. The end result is the same - the composition of the gastric juice changes, its acidity increases or decreases, excellent conditions are created for the reproduction of pathogenic microorganisms, atypical cells can begin to form, which subsequently lead to the appearance of malignant formations of the stomach and esophagus.

Pediatric gastritis usually occurs at the age of 4-6 years or later, in school-age children.
Experts say that the fault is unhealthy diet, the bad habit of parents to feed the child for any reason with a variety of pills, the prevalence and popularity of fast food, as well as a significant deterioration in the ecology and quality of food.


However, recently, more and more often the disease is found even in infants.who still have no idea what a hamburger is, what they eat it with. Their stomachs suffer from the quality of the infant formula, the frequent experiments of the parents to change the formula and during the introduction of complementary foods.

Classification
According to the duration of the pathology, gastritis is acute and chronic:
- Acute form. It develops quite rarely, it is always a quick reaction of the body to an aggressive factor. This can happen if a child has eaten food contaminated with pathogenic bacteria, if he has swallowed something poisonous, toxic. Sometimes acute gastritis is a reaction to certain viruses that can survive in an aggressive environment of gastric juice (for example, rotavirus). This condition may be preceded by the intake of certain medications that injure the delicate inner lining of the children's stomach.

The severity of the condition depends on the subspecies of acute gastritis. Catarrhal - the simplest, arising as a reaction to poor-quality food. Fibrinous (erosive) - quite severe, it becomes a consequence of acid poisoning. The most difficult is necrotizing gastritis. They talk about it in case of severe acute poisoning with concentrated acid, heavy metal salts, it leads to the death of stomach tissues.
- Chronic form. Among all established diagnoses of gastritis, chronic gastritis accounts for more than 80%. The disease becomes a sad reality with prolonged negative effects on the digestive system. The most unusual is autoimmune gastritis, its mechanism is similar to an allergic reaction. Immunity attacks the cells of its own body, mistaking them for hostile - due to antigen proteins.

The most common subspecies of chronic gastritis is infectious or bacterial.
Such an ailment (according to scientists) is caused by the notorious microbe Helicobacter pylori. He is also guilty of inflammation of the duodenum along with part of the stomach. This disease is called gastroduodenitis.

Another subtype of the disease is reflux gastritis, a condition in which bile acids are injected into the stomach, which causes inflammation. In case of radiation sickness, the destruction of the inner shell by primary radiation sickness.
Causes
The acute form of the disease in children is caused by quite certain factors. These are expired products in which bacteria multiply, and chemicals that, through an oversight of a parent, a child can taste, and poisons. A chronic disease has much more probable causes:
- Helicobacter pylori. The microbe, whose name is so widely advertised by manufacturers of drugs for heartburn, is considered the main "culprit" of gastric problems. It was revealed only in the second half of the 20th century. His "father" is Australian physician Barry Marshall. To prove his theory of the relationship between bacteria and diseases of the digestive system, he infected himself with this microbe, for which he was awarded the Nobel Prize in Medicine in 2005.

Official medicine believes that in patients with gastritis, this microbe is found in 80-90% of cases, however, in people infected with Helicobacter pylori (and there are 9 out of 10 people on the planet), gastritis does not always develop.
Apparently, there are still "blank spots" in Dr. Marshall's theory.
- Duodenogastric reflux. This is the cause of chronic gastritis in the event that the contents of the duodenum are regularly thrown into the stomach and irritate it.

- Eating disorder. This reason was considered the main one before the discovery of the bacterium Helicobacter pylori, now it is the second most likely, in any case, the doctor will never discount this factor. A violation is understood as an irregularity of food intake, an imbalance of nutrients, a chronic lack of vitamins and trace elements, as well as the consumption of foods that a child (due to the immaturity of enzyme metabolism) is still difficult to digest normally - fatty, fried, pickled, spicy, exotic.


- Taking medications. If a child takes drugs for a long time that can irritate the gastric mucosa, the likelihood of chronic gastritis increases. These drugs include some hormones, non-steroidal anti-inflammatory drugs, drugs containing acetylsalicylic acid.

If these medications are prescribed by a doctor for another disease, he will certainly take into account the possible risk, calculate the dosages and draw up a treatment schedule in which the effect of medications on the children's stomach will not be so destructive.
It is much worse if the parents "treat" the child at their own discretion and give him various pills and syrups when they see fit.
- Parasites. Various parasites that feel great in the child's body, helminthic infestations can also cause chronic gastritis, since for a long time they parasitize in different parts of the intestine, disrupting metabolic processes and "throwing" their own waste products into the child's bloodstream. It is this “waste” that is dangerous.

- Stress. This factor explains why children of primary school age or older adolescents begin to suffer from gastritis most often. They are characterized by the accumulation of stress, chronic stress. In the first group (6-7 years old) this is associated with drastic changes in life in connection with the beginning of school attendance. In the second group - nervous factors associated with puberty, first falling in love, high academic load at school.


- Other reasons. Chronic infectious diseases, hereditary risk factors, as well as food allergies that were not detected in time, so the child continued to eat a product that caused negative changes for a long time, can also be considered as possible causes of gastritis in children.
The rash that accompanied this process could be attributed by parents to anything - to another allergy, to prickly heat or an infection. How they were treated does not matter, the main thing is that the product remained in the diet, and the allergy continued to flow.


Factors that increase the likelihood of this unpleasant and intractable disease in a child include iron deficiency in the blood, metabolic disorders and thyroid disease, kidney failure, and heart disease.
Symptoms and Signs
Acute gastritis of a catarrhal course by external signs often resembles food intake in the broad sense of this term.
The child first loses his appetite, then his stomach begins to ache, the pain is dull and is localized just below the solar plexus. Then vomiting, diarrhea may open. Symptoms change quite quickly, and it can take only half an hour or an hour (or a little more) from refusing to have dinner to a state of vomiting and diarrhea.

If acute gastritis is caused by poisons, chemistry, acid drunk, then the course will be faster and more intense. The first symptom will be a sharp pain in the stomach, the appearance of temperature, fever is possible. Almost simultaneously or with a difference of half an hour, severe frequent vomiting develops, possibly with blood impurities. Blood can also be observed in the stool if the child has diarrhea. A state of dehydration develops very quickly, which is extremely dangerous and can be fatal.
Vomit with toxic acute gastritis has a pronounced chemical or acid odor, and the breath smells the same. The general condition is serious, urgent medical attention is needed.
Signs of chronic gastritis are much more difficult to recognize, especially at an early stage:
- Feeling of heaviness "I swallowed the brick." The child most often experiences it immediately after eating. But he does not always complain of a strange sensation.

- Vomiting and nausea... These signs accompany the baby not every day - and not even every week. And signs of episodic nausea do not always force parents to run to see a doctor.
- Heartburn... The symptom is quite characteristic, but children up to 11-12 years old are simply not able to describe in words this condition in which gastric juice is thrown into the esophagus, and therefore the parents simply do not know about it.
- Decreased appetite... This symptom in itself cannot speak of the presence of gastritis, since the child's poor appetite is the scourge of so many parents. If the child has always eaten well, but for no apparent reason has been refusing food for several days and is clearly unwell, it is better to show him to the doctor.
- Stool problems... Children with developing chronic gastritis have pronounced delicate problems: diarrhea alternates with constipation - and vice versa. Normal stool is an exception for them.

- Rumbling in the stomach... It is rather difficult to determine the presence of gastritis only on this basis, since all people (even completely healthy ones) rumble from time to time, gurgle and gurgle in the stomach. The frequent occurrence of such sounds should alert parents. If your stomach growls several times a day, this is a reason to go to the doctor's office.
- Weight loss... If the gastritis is already long enough, then the child can lose weight for no apparent reason.
In a state of exacerbation, chronic gastritis manifests itself as acute - vomiting of food eaten, a slight increase in temperature, slight pain in the stomach, diarrhea, signs of general intoxication.
Diagnostics
Acute gastritis is diagnosed urgently, according to the totality of symptoms. With chronic, things are more complicated. After contacting a pediatrician with complaints about one or more symptoms from the above list, the pediatrician will definitely give a referral to a gastroenterologist.

This specialist cannot say anything about the appearance of the child alone, you need to go to him, having on hand the results of laboratory tests and other studies:
- Gastroscopy... This is a method that allows you to visually assess the condition of the walls of the esophagus and stomach. The EGDS procedure is performed using a special device - a gastroscope. It is introduced into the esophagus through the larynx, sometimes the study is accompanied by a biopsy, taking tissue fragments for analysis.

- Gas analysis... Using a gas analyzer, the ammonia content in the exhaled air is checked after taking urea. This method allows you to establish whether the body has that very amazing Helicobacter pylori bacteria.
- Ultrasound... On an ultrasound examination, the diagnostician will assess not only the condition, size and characteristics of the stomach, but also the condition of all organs of the abdominal cavity. This will make it possible to judge the degree of damage that gastritis could cause.

- Analyzes blood, urine, feces, including blood and feces tests for Helicobacter pylori.
Treatment
In case of acute gastritis, you need to call an ambulance - and at the same time begin to provide first aid to the child. It consists in giving the child plenty of warm water and to induce vomiting. This procedure, carried out several times, allows you to cleanse the stomach cavity from aggressive substances or low-quality food.
In a hospital setting, a tube will be inserted into the child's stomach and it will be washed professionally and skillfully. On the first day, food is prohibited. Then, other products are gradually introduced into the child's diet that will not irritate the esophagus and mucous membranes (soups, porridge-spreads, jelly, white bread croutons without salt and spices).
With severe pain, the child is given antispasmodics. The intake of enterosorbents ("Smecta", "Enterosgel") is always shown. With severe acute gastritis, the baby is hospitalized in the intensive care unit, where (in addition to the above measures), saline and glucose will be injected intravenously to relieve the symptoms of dehydration, as well as potassium preparations.


Chronic gastritis is more difficult to cure, therapy takes longer and requires strict adherence to the recommendations of specialists.
First of all, the nutrition is adjusted. The child is assigned a diet appropriate to the degree and nature of the disease. It is recommended to eat fractionally - 4-6 times a day, in small portions.
All spicy, salty, pickled foods and canned foods, spices, fried foods are excluded. Depending on the degree of gastritis and the level of acidity of the gastric juice, the doctor may prohibit eating sour fruits and berries or recommend moderately acidic foods if the acidity is insufficient.
Prohibited:
- grapes;
- chocolate;
- coffee and cocoa;
- all lemonades and carbonated drinks without exception;
- shop baked goods, factory sweets;
- sweet tea;
- black bread;
- everything smoked, fatty and fried.

The menu for the week (especially at first) is best coordinated with the attending physician. Then proper nutrition will be carried out out of habit.
Medical treatment is selected strictly individually.The most common treatment regimens include drugs that make it easier for food to pass through the esophagus and relieve spasms. This is usually No-shpa or Papaverine. In case of insufficient acidity in the stomach, the drug "Abomin" can be prescribed, with excess - "Almagel", "Maalox", "Fosfalugel". To normalize gastric motility, "Motilium" is prescribed.
When Helicobacter pylori is identified as the main "culprit" of the disease, antibiotics can be prescribed, a specific drug is selected by the doctor, based on the child's age and the characteristics of the course of his disease.

Quite often, doctors prescribe two antibiotics at the same time - "Clarithromycin" and "Amoxicillin", since it is this "duet" that shows the best results in the elimination of Helicobacter pylori. But this therapy itself is controversial. Considering that the bacterium is extremely widespread, the likelihood of "picking up" a new one instead of the destroyed one is very high. The microbe is perfectly transmitted by kissing, with saliva, through raw water, dishes, and enters the body through dirty hands.


If the doctor does not prescribe pills to the child, there is no professional oversight in this, as it might seem to the parents.
The fact is that in children under 12 years of age, moderate forms of chronic gastritis are perfectly amenable to correction with the help of diet and physiotherapy alone. Only if these measures do not bring positive changes, the doctor will consider prescribing medication.
Forecasts
Catarrhal acute gastritis in most cases has a favorable prognosis. This, unfortunately, cannot be said about acute toxic (necrotic) gastritis, in which the first 2-3 days are considered life-threatening. Much depends on the timeliness of the assistance provided to the child, including first aid before the arrival of the doctor. If life is no longer threatened, the prognosis improves slightly, because changes in the inner gastric membrane are significant, they often lead to scarring of tissues and the development of atrophic gastritis, which remains for the rest of your life.

An unfavorable prognosis in chronic gastritis. The only exception is the superficial form, since only it has the possibility of reverse development. All other chronic gastritis, as a rule, remain with a person for life. But with proper and timely supportive treatment, adherence to a diet, and limiting stress, periods of remission are long, and the child may well lead an ordinary life.
The chronic form of atrophic gastritis has the most unhappy prognosis - it often turns into stomach cancer.
Experts believe that the most favorable prognoses have forms of pathology, accompanied by normal or high acidity. With a reduced risk of developing more serious complications, it is significantly higher.
The child must definitely visit a doctor (at least 2 times a year), take tests and undergo examinations so that the doctor has a clear idea of whether the disease is progressing and at what rate, and can correct the treatment regimen in a timely manner.
Prevention
Gastritis is a disease that is easier to prevent than treat.
Therefore, it makes sense to engage in prevention from a very early age:
- The gastric mucosa has direct contact only with air and food (water). Therefore, it is important for the child to eat properly. The baby should be given complementary foods according to pediatric standards; older children should not be given foods that can cause an allergic or toxic reaction. Particular attention should be paid to the quality and freshness of the food.
- The child's diet must be formulated correctly and reasonably. It should not contain fast food, there should be an alternation of first courses and thicker foods. The rule “not a day without soup” should be written in big letters in the kitchen of every mom who wants to raise her child healthy.

- Don't skip meals. For the stomach to function properly, it is very important that food comes in small quantities and at regular intervals.
- It is useful to teach the child to chew food for a long time and patiently, to eat not in front of the TV, but at the table, since eating in front of the screen usually leads to a banal overeating.
- The child must learn to wash his hands every time he goes to the table.
- All chemicals hazardous to the child, household chemicals, solvents and acids needed by the parents in the household should be out of the baby's reach. Otherwise he might taste them one day.
- You shouldn't give your child different tablets and syrups every time you feel unwell. Headache, toothache, abdominal pain and other symptoms are a reason to visit a doctor, and not go to the pharmacy for a pill for a child.
- An active lifestyle, playing sports, hardening, strengthening the immune system are excellent preventive measures. However, with physical exertion, you need to be more careful with those who have already found chronic gastritis, since overwork can exacerbate the disease.
For information on how to eat right with gastritis, see the next video.



