The middle of pregnancy is the most beautiful time. The expectant mother is not yet tired of her "interesting position", but she has already managed to enjoy the period of waiting for the baby. It is during this period that the second planned examination falls, which is called the second trimester screening. It includes ultrasound diagnostics and a biochemical blood test. What the baby can show on an ultrasound scan at this time and how to decipher the examination protocol will be discussed in this material.


Why is this needed?
Ultrasound examination in the second trimester is part of the screening, the task of which is to identify the increased risks of having a child with genetic and other pathologies and abnormalities. By order of the Ministry of Health of Russia, studies that are carried out in the first and second trimester, are considered mandatory. Women pass them free of charge in a consultation at their place of residence


The indicators that the ultrasound diagnostics doctor receives are processed with the help of a special computer program together with the results of a blood test, in which hormones and proteins are determined, the level of which may indicate possible pathologies in the child and bearing problems.
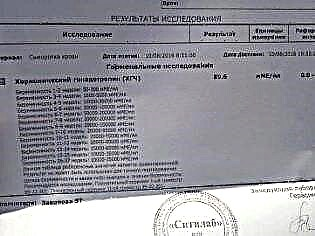
In the first trimester, the content of hCG and PAPP-A protein is established in the blood, in the second, the so-called triple test is performed - hCG, estriol, alpha-fetoprotein.
The program "brings together" the data obtained from two sources, analyzes individual risks - the woman's age, the presence of bad habits and chronic diseases, the facts of the presence of genetic pathologies in the families of the future mother and father, and gives a result that indicates how likely a given woman will have a child with Down, Edwards, Patau syndromes and other incurable and even fatal pathologies

First trimester screening, which takes place from 10 to 13 weeks, considered the most informative. The second study gives much less information on markers of genetic pathologies, but it allows the expectant mother to see her fairly grown baby on the monitor of an ultrasound scanner, to find out how the baby is developing, and also to clarify the sex of the child. It is in the second trimester that it is easiest to determine gender on an ultrasound scan.


The child is not yet so big as to shrink into a lump and thus close the view of intimate places, but not so small as not to see the formed genitals.
Features:
The timing of the second scheduled ultrasound scan is not as tight as in the case of the first screening study. The Ministry of Health recommended that the examination be carried out in the period from 18 to 21 weeks. In practice, these terms can be shifted both up and down. Often, a pregnant woman is sent for screening at a period of 16-17 weeks; periods of 10-24 weeks are also considered quite common and popular among obstetricians-gynecologists.


Not so long ago, they might not have been sent for a second scheduled ultrasound if the first screening showed results that did not cause concern for the attending physician. The second ultrasound scan was mandatory for women at risk - pregnant women over the age of 35, women who had already had children with genetic pathologies and some other categories of expectant mothers. Now the second examination is carried out by all, without exception, and therefore do not worry if the doctor gives a referral for a second screening examination.


An ultrasound scan in the second trimester is performed in order to identify:
the number of children (it happens that during the first examination the second fetus is not visible and opens to the doctor's eyes only on the second examination);
the position of the crumbs in the uterus, its estimated weight, height;
the sizes of the limbs, head, abdomen of the baby separately (the development of each part of the body is of great importance for determining the proportions and characteristics of the baby's development);


the heart rate of the child and the structural features of his heart;
structural features of the facial bones, chest, spine;
structural features of all important internal organs - kidneys, liver, lungs, brain);

the amount of amniotic fluid (water surrounding the baby);
degree of maturity, thickness and location of the placenta;
condition of the cervical canal, cervix, presence or absence of tone of the uterine walls.


If the gender of the baby is not yet known or the results of the first ultrasound are in doubt among the parents, then now is the time to ask the doctor an interesting question about who "lives in the belly" - a boy or a girl. But you should know that determination of the child's sex is not included in the standard examination protocol, therefore the doctor has the right to refuse this request or you will have to pay for this service. Many consultations have officially included the determination of the baby's sex in the list of paid services.

The very procedure of ultrasound examination is carried out by the transabdominal method - through the abdominal wall. However, in some cases, the doctor uses the transvaginal method. It is easier for a vaginal sensor to get a clearer image of the baby if the mother has an extra weight, a dense fat layer on the abdomen that makes it difficult to visualize through the peritoneum. Sometimes both methods of research are used at once.
The diagnosis takes about 10 minutes and is painless and completely safe for both the woman and her baby.


Preparation for research
If before the first ultrasound the woman was advised to prepare - to empty the intestines before visiting the doctor's office, including from accumulated gases, then no specific preparation is required before the second scheduled ultrasound. Even if there are accumulations of gas in the intestines, then this will not have any effect on the ultrasound results. The uterus that has grown in size pushes the intestinal loops into the background.
There is also no need to fill the bladder.

You can eat anything before the study, but just before entering the ultrasound room, a woman can eat a small chocolate bar. A tiny person inside her will quickly react to sweets and begin to move more actively, which will allow the doctor to assess the baby's motor functions and better examine him in different projections.


By agreement with the diagnostician, you can take the father of the unborn child with you for the second ultrasound scan. Something quite interesting awaits him on the scanner monitor, because now the fetus is clearly visible, you can admire its profile, see the arms and legs, fingers, nose, mouth, eye sockets, genitals. If the ultrasound is done in 3D, then future parents will even be able to see who the toddler looks like more.


After the procedure, the woman is given a research protocol in which she will find a lot of abbreviations and numerical values. Not every doctor in a consultation has the opportunity to tell every expectant mother in the process of diagnostics what this or that indicator means, what he is talking about. Therefore, you will have to understand the jumble of numbers and letters yourself. We will help you with this.
Decoding the results
By the second trimester, a woman had already perfectly learned that there is a period that she calculates herself (from the moment of conception), and there is a generally accepted obstetric term - it is customary to calculate it from the first day of the last menstruation. Doctors of ultrasound diagnostics, as well as obstetricians-gynecologists, use obstetric terms, therefore, all data on the correspondence of parameters to certain terms are indicated in terms of calculation (day of conception + about 2 weeks).


Fetometric parameters of the fetus that are looked at by ultrasound and described in the protocol include the following.
BPR (biparietal size)
This is the distance between the two parietal bones. It is this indicator that is considered the most informative in determining the exact duration of pregnancy in the second trimester. If it does not meet the deadline, this may be a symptom of a delay in the development of the baby.

LZR (frontal-occipital size)
This distance, which is the segment between the two bones of the skull - the frontal and occipital. This indicator by itself is never evaluated and does not say anything. It is considered only in conjunction with the above-described BPR. Together, these measurements indicate gestational age.


Table of BPD and HPR in the second trimester:
If the size of the head differs slightly from the norm of indicators to the smaller side, then this may be due to the constitutional characteristics of the fetus - mom and dad may have small skulls. However, if BPD or LHR is significantly behind (more than 2 weeks from the actual period), the doctor may have questions about the development of the child - is there a developmental delay, whether the baby has enough nutrients and vitamins.

A decrease in these indicators often happens in pregnant women who, while carrying a baby, could not say goodbye to bad habits (alcohol, smoking), as well as during pregnancy with twins or triplets. The ratio of BPD to the rest of the fetus is important. If the head is reduced proportionally and other sizes also do not reach the lowest threshold of the norm, then we can talk about both a constitutional feature (a thin child) and a symmetrical developmental delay.
If the rest of the parameters are normal and only the head is reduced, additional examinations will be prescribed, including ultrasound in dynamics, in order to exclude brain pathologies, microcephaly and other abnormalities.


Exceeding the upper threshold of standard values, if it is symmetrical to the rest of the baby's size, may indicate an error in calculating the term, for example, due to late ovulation, or a tendency to a large fetus. An asymmetric enlargement of the baby's head needs a separate examination, since it can talk about dropsy of the brain, about other disorders of the central nervous system that caused swelling of the brain.
OG (head circumference) and coolant (abdominal circumference)
The size indicating the circumference of the head is important in assessing the development of a child. The gestational age for this parameter is not separately calculated, the OG is considered in relation to the BDP and LHR (mainly to understand the head proportions). The baby's head grows most actively in the second trimester, and therefore this size is rapidly changing.


OG table - second trimester (average norms and permissible deviations):
Exceeding the exhaust gas norm for 2 weeks or more will require additional examination, since it may indicate hydrocephalus. A slight excess may be due to an error in the calculation of the obstetric term. A decrease in TG below the permissible norm for more than 2 weeks indicates intrauterine growth retardation, if other parameters of the child's body are also reduced.
If only the head is less than the norm, the child will be examined for pathologies in the development of the brain and central nervous system.


Abdominal circumference is an important parameter that helps the doctor to clarify the condition of the child if developmental delay is suspected. Most often in the second trimester there is a form of delay in which the proportions of the baby are not symmetrical. In other words, not all measurements indicate a decrease. In this case, the lagging standards are compared with the abdominal circumference in order to understand whether there is a pathological lag, or thinness and small stature is a hereditary characteristic of a particular child.
Coolant table in the second trimester:
Slight lag behind average values not considered pathological the close attention of doctors deserves a situation when the circumference of the baby's tummy lags behind the norm by more than 2 weeks. In this case, the parameter is compared with BPD, OG, LZR, as well as with the length of the baby's limbs, and the umbilical cord and placenta are also examined in order to exclude oxygen starvation and insufficient nutrition of the child.
The deviation of this parameter alone, if all the others correspond to the gestational period, does not mean anything alarming, it is just that babies in the second trimester grow in leaps and bounds.
It is quite possible that after a couple of weeks at an extraordinary ultrasound scan (and he will be appointed to double-check the data), the "norm" will be indicated in the coolant column.


Bone length
In the ultrasound examination protocol, these dimensions are indicated as follows - DBK (length of the femurs), DCG (length of the shin bones), DCP (length of the forearm bones), DPC (length of the humerus), DKN (length of the nasal bone). All these bones are paired, therefore, the protocol will indicate double numerical values, for example, DBK - 17 left, 17 right


The length of the limbs in the second trimester is a marker of genetic disorders. For example, many incurable syndromes (Patau, Cornelia de Lange and others) are characterized by shortened limbs. Although, of course, no one will judge the norms and deviations so unequivocally. Suspicions should be supported by negative results from the first screening, as well as biochemical blood tests.


Often, deviations in the length of paired bones are observed in girls, because they develop at a different pace, and in most cases have more miniature parameters than boys, and the tables used by doctors to check ultrasound data are compiled without regard to gender.
DBK (length of the femurs) in the second trimester:
DCG (the length of the shin bones) in the second trimester:
Duodenum (length of the humerus) and PrEP (length of the forearm bone) in the second trimester:
The length of the nasal bone in the second trimester is not as important as during the first screening. It can no longer be considered a marker indicating a possible Down syndrome in a child. By the middle of pregnancy, the baby's nose has the size and proportions that are laid in it by nature, and this size is individual. In some consultations, doctors the second ultrasound does not even measure the nasal bones, but simply indicate in the protocol that these bones are visualized or write that the bones of the nose are normal.
Nevertheless, expectant mothers who have numbers in the "Nasal bones" column in the ultrasound protocols will be interested to know how "nosed" their child will be.

The average size of the nasal bones of the fetus in the second trimester:
Internal organs, face and brain
If gross malformations are not observed in the baby, the diagnosticians do not go too deep into the description of the internal organs of the baby. In the received protocol, the expectant mother will be able to see just a list: the kidneys are normal, the heart has 4 chambers, and so on.
If pathologies are noticed, then the type of the detected anomaly will be indicated in the corresponding column, for example, a formation of the "cyst" or "underdevelopment" type.


Assessing the state of the brain, diagnosticians note the size of the lobes, their outlines, the structure of the ventricles, the size of the cerebellum. The facial bones at 5 months of pregnancy are well formed, and the doctor can easily examine the eye sockets, measure them, make sure that the baby's upper and lower jaws are normally developed, and also note, if any, clefts - the so-called cleft palate and a cleft lip.
When examining the spine, the doctor will assess its general condition, examine it for possible clefts. When diagnosing the lungs, the doctor will note the degree of their maturity, in the second trimester it is normally the third
Placenta
The location of the "child's seat" is of particular importance.The most common location is on the posterior wall, although anterior dislocation is not considered an anomaly. The location of this temporary organ feeding the baby influences the choice of tactics of childbirth. For example, a low position or dislocation along the anterior wall of the uterus may be a prerequisite for the appointment of a planned caesarean section.
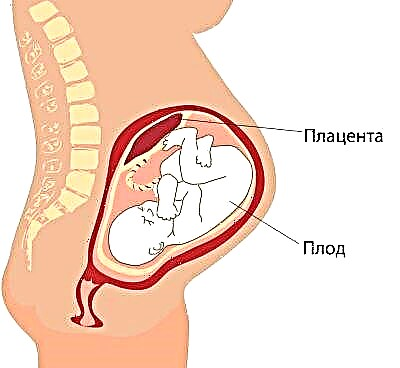
Low placentation is established when the "child's place" is located below 5.5 centimeters from the internal pharynx, but if this temporary organ overlaps the pharynx, in the conclusion indicate that there is a placenta previa. In no case should this cause panic in a pregnant woman, because as the uterus grows, the placenta can rise higher, and often this happens already towards the end of gestation and is confirmed by an ultrasound examination in the third trimester.


In addition to location, the doctor reveals the thickness of the "child's seat" and the degree of its maturity. The normal thickness for the middle of pregnancy is considered to be a value of 4.5 cm.If the placenta turns out to be thicker, an additional examination is prescribed, since such an increase in the temporary organ can indicate pathological processes, for example, the development of the Rh conflict between the mother and the fetus, as well as some genetic disorders , intrauterine infections.
The maturity of the placenta in the second trimester should be zero. If the doctor assesses it as the first, we can talk about the premature aging of the "child's place", the loss of some of its functions and the potential danger to the child. At the same time, the thickness also changes - the placenta becomes thinner, usually with early aging in the middle of pregnancy, its thickness is estimated at 2 centimeters or less.
Before 30 weeks, the placenta should ideally be at zero maturity. From about 27 weeks, she can become the first, and from 34 - the second. By childbirth, this organ “grows old” to the third degree.
Amniotic fluid (water)
Transparency, presence or absence of suspension, as well as the amount of water surrounding the child inside the fetal bladder, is of great diagnostic value. The ultrasound protocol indicates the amniotic fluid index, which gives an indication of whether the amount of water is normal. Polyhydramnios and low water may indicate that the baby has pathologies, that an infection has occurred. These conditions necessarily require medical supervision, supportive treatment and the choice of the correct tactics for the delivery.


Average rates of the amniotic fluid index (AFI) in the second trimester:
Umbilical cord
The study of the umbilical cord gives an idea of how the baby is supplied with oxygen and nutrients, in addition, the pathology of the structure of the connecting "cord" may indicate possible genetic pathologies in the child.
Usually normal a healthy umbilical cord has 3 vessels, two of which are arteries and one is a vein. It is through them that the exchange between a woman and a child takes place. The mother supplies the baby with nutrition and oxygen, and the baby "sends back" unnecessary metabolic products that are excreted through the mother's body.


An insufficient number of vessels may indicate a possible development of Down syndrome in a child, but is not a mandatory marker. Sometimes the absence of one artery in the umbilical cord is compensated by the work of another artery, and the child is born healthy, albeit with reduced weight.
The presence of only one vessel is a sign of fetal pathologies, and here a detailed genetic study and invasive diagnostics are required.


At the conclusion of the ultrasound, the expectant mother, thus, will see the number of umbilical cord vessels found by the doctor, as well as a mark that the blood flow through them is normal (or there is a decrease in its speed).
Uterus
The doctor on the ultrasound is interested in whether the pregnant woman has a threat of termination or premature birth. Therefore, he assesses the presence or absence of tone of the uterine walls. If a woman has previously undergone a cesarean section or other operations on the genital organ, it is necessary to evaluate the consistency of the postoperative scar.

If everything is in order with him, then the ultrasound examination protocol indicates that the scar has no features, and the thickness of the scar tissue is also indicated. Features include niches, thinning of the scar, which creates the risk of rupture of the uterus and death of the fetus and mother.
In addition, the cervix and the state of the cervical canal are described. This shows if there is a threat of miscarriage or premature birth.


Final part
In the final part of the protocol, it is indicated whether the fetometry data correspond to the obstetric term. The size of the fetus allows using several formulas to calculate its estimated weight. The actual weight may differ from this value with a fairly large error. The weight is calculated by the program installed in the ultrasound scanner. If your consultation has old-style equipment installed, there may not be such a point in the protocol at all.


Fetal weight (average) in the second trimester:
16-17 weeks - 50-75 gr.
18-19 weeks - 160-250 gr.
20-21 weeks - 215-320 gr.

22-23 weeks - 410-490 gr.
24-25 weeks - 580-690 gr.
26-27 weeks - 800-910 gr.
28 week 980-1000 gr.

Common questions
After IVF
For women who become pregnant with IVF, ultrasound diagnostics is performed a little more often, therefore, in the second trimester, they are not waiting for the second, but the fourth or fifth ultrasound. In relation to such expectant mothers, they try to conduct the research more carefully, in their conclusion there will be information that is not entered during the standard procedure - determination of the blood flow velocity through the uterine and placental vessels. It is important to understand if the baby is doing well "out of the test tube".


When pregnant with twins (triplets)
In this case, ultrasound examination of the second screening implies a detailed description of each of the fetuses. Do not be afraid that the parameters of babies will be different, because two or three little people cannot develop according to the same scheme, despite the fact that they are carried by the same mother.


Inability to determine gender
If the doctor at the second ultrasound was unable to tell the parents the sex of the future baby, this does not mean that the study was carried out poorly. This is rare, but it is possible that at the time of examination, the baby just took an uncomfortable position for review or turned his back to the sensor.
In this case, the specialist cannot guarantee an accurate result.